Botanical Therapy
For the Nervous System
GOTU KOLA
Welcome to our deep dive into the nervous system, which for sure includes some of our most beloved plant allies! I have spent decades working with plants to support people’s stress, anxiety, depression, and mental health. I’ve learning a lot about the plants that help us acutely when needed day to day, as well as tonics that can transform our mental and emotional realms pretty powerfully. We covered this system very in depth in year one, so please use both modules to complete our look at the nervous system. For this second year, I’ll focus now on addressing specific illnesses of the nervous system more directly, and how to recommend herbs safely at the most effective doses.
Plants that support our nervous system are daily remedies. I build my herbalism practice on nourishing herbs and adaptogens as the base, and then nervous system support. I am often cycling through plants that support different organs of my body I can feel need tending to, but stress relief and calming nervines are a must every day. When I recommend herbs to others, nervines are a constant. We all need nervous system support… whether it’s with stress, depression, anxiety, sleep, mental focus, or to just support relaxation. Humans and many animals have always needed plants to support our nervous systems. We have always used alcohol, smoking, and many drug like plants… but they often come with a host of other difficult side effects. Nervines are a safe and effective alternative to bring us the ease we need daily. They can be especially helpful when we have a history of needing Western drugs or recreational drugs to calm ourselves through emotional or mental stress.
The human brain and nervous system is difficult to manage, and brings us an often more challenging life than other animals (in the wild). I think stress relief and emotional support is more than half of what’s needed every day in terms of healing therapies for humans. It takes effort and care to keep ourselves emotionally and mentally well in an unwell society. Our whole body and being needs ease and peace in a society constantly blasting our mind and nervous systems. It takes wisdom, discernment, and very strong boundaries to create peace and calm within. Plants are powerful healers for our mind and emotions. Tending to ourselves and receiving the support we need allows us to support the communities around us better. Through connection and intimacy with plants and nature, we’ve found deeply important medicine needed for the illnesses of human society.
An important thing to note as well… When people are going through physical or emotional illness, it is stressful. Illness in general can cause a lot of anxiety, depression, worry, and a range of emotions. It’s not easy to experience sickness that’s more than just a cold or flu. Chronic illness always comes with a level of stress that needs support. I also include mental and emotional suffering to be in the category of chronic illness, since dealing with emotional and mental suffering, as well as the effects of trauma (which is all to0 common) is similar to tending our physical body through a long term illness.
Sometimes we need these emotional support plants most during times of intense struggle, and when that period passes we need them less frequently. If someone is dealing with a period of immense struggle and stress they need a lot of tending to for that period of time, and then the need will naturally change once things shift. Most suffering is relieved in time, generally it is temporary and will not last forever. These plants can create real moments of relief when we need it, and our role for others can be offering the acute help someone needs.
Spend time considering what challenges of the mind and nerves you see most in your communities. What do you see people most needing? What would you like to support in those who surround you? I see a lot of overwhelm, over focus on work, busyness, stress, distraction, depression, insomnia, irritability, emotional swings, and high anxiety/panic. Our happiness level seems to continually be going down even with so many of our basic needs met. We all have to consider what really contributes to emotional wellness, and what is causing our suffering. Explore plants (and dosages!) that help to relieve anxiety, calm the mind, relax tension in our body, ease pain, and help us sleep deeper. Make friends with the adaptogens that can regulate our stress response and help rebuild the nervous system. Remember the power of our nourishing herbs like oatstraw and nettles to stabilize the nervous and endocrine systems, strengthen our adrenals, and regulate our energy levels.
OATSTRAW
I hope this module also helps you to feel more confident recommending plants to help relieve suffering and bring mental peace. I hope you get to know more of these amazing plants that support our well being. Choose a few more plants to explore! Use them in different preparations and get a strong sense of how each feels in your body. The plants in this module are needed by all of us, and daily in my opinion. Learn the plants in your own body. Explore how skullcap feels as a tea, tincture, and glycerite… Feel the taste of ashwagandha infused in honey, or blended with burdock in tea. Learn how to brew a good peony root tea that isn’t too strong, and play with doses of blue vervain tincture. Feel their effects at different doses, notice what the nervines feel like at stronger doses, or teas vs. tinctures. You have to learn each plant through different preparations, concentrations, and dosing. Experimentation is the path to learning with herbalism. Start with weaker doses and work your way up feeling the difference.
Many of our dream activating nervine plants open the 3rd eye, which allows us to experience more of our lives and the divine world around us in a deep way! Consciousness shifting plants bring us beyond our limited perceptions, opening us to the realms of nature and spirit… Many of the plants we talk about this module rewire the brain and nervous system to allow new experiences and awareness in. Visioning plants can bring us sight beyond just what our eyes can see! They increase our sensory experiences and create new neural pathways. Plants are awakened beings that can help us experience more of life and the universe… allowing us to vision and see what is possible.
Remember the plants are the ones doing the work, we are just helping bring them to more people. Reminding our communities of the medicine that literally surrounds us all. Plant medicine belonged to all of us once, and one day it will again. The plant elders are wise healers, and they will be available to call on to support your community for many years to come.
May these plants help your heart and mind awaken to peace,
In peace and ease,
Sage
Video ~ Nervous System
& Third Eye Welcome
The Nervous System
The Brain, Neurotransmitters, and Nerves
We will now move on to discussing plants that support the health of our physical brain and nerves. There is a lot we can do to support the health of our nerve cells, reducing damage and stimulating repair. Science has also now shown us that every organ in our body produces neurotransmitters, which are communicating with our nervous system constantly. This just illustrates the truth that our whole body is communicating, and our nervous system (mind, nerves, and heart) are picking up information constantly.
For all of us there are always multiple factors to what we are feeling mentally and emotionally… layers of feeling, emotions, sensations, thoughts, and memories coming from all parts of our body and being. If we don’t rush, with curiosity and patience we can discover slowly what’s happening within and what might be needed for support. It’s important to focus on multiple therapies and practices that will strengthen and nurture someone’s mental and emotional health both on a physical level and beyond…
Aspects of Nervous System Health
9. Reducing causes of damage to nerve/brain cells (reduce exposure to toxins and introduce antioxidants like clove, cinnamon, turmeric, sage, basil, rosemary, fruits, blueberry, pomegranate, hibiscus, rose hips).
~
10. Stimulating repair of nerve tissue (nerve repair herbs like st. john’s wort, skullcap, oatstraw, mimosa, butterfly pea, gotu kola, and ginkgo).
~
11. Rebuilding nerve myelin sheath (silica rich plants like nettles, oatstraw, and horsetail).
~
12. Supporting brain repair (herbs like lion’s mane, ginkgo, schisandra, siberian ginseng, gotu kola, ashwagandha, bacopa, astragalus).
~
13. Circulation & oxygen to the brain (herbs like ginkgo, rosemary, gotu kola, and schisandra).
~
14. Repairing fatty tissue around nerves (omega fatty acids in fish oil, primrose oil, borage oil, olive oil, hemp oil, flax, and chia).
~
15. Repairing damaged DNA in nerve/brain cells (herbs like reishi, astragalus, and siberian ginseng).
~
16. Repairing musculoskeletal pain and injury effecting nerves tissue. Including tissue inflamnation or cramping. (turmeric, ginger, comfrey, arnica, st john’s wort, plantain, black birch, evergreens, as well as antispasmodics like kava, cramp bark, valerian, peony, magnolia.)
1. Nourishing nutrient deficiencies (herbs high in calcium, magnesium, B vitamins etc. like nettles, dandelion, and oatstraw).
~
2. Healthy gut bacteria (probiotics, fermented vegetables and inulin rich herbs like burdock root, dandelion root, elecampane etc.)
~
3. Support deeper sleep (sedatives like skullcap, mugwort, california poppy, blue vervain, passionflower, valerian).
~
4. Endocrine and hormonal balance (using adaptogens like ginseng, schisandra, and ashwagandha as well as other endocrine tonics like chickweed, nettles, oatstraw).
~
5. Sedating or calming nerves (all of our wonderful nervines like peach, blue vervain, california poppy, skullcap, oatstraw, linden, catnip, lemon balm, lemongrass, soursop/guanabana, motherwort, passionflower, kava, mugwort, rose etc.)
~
6. Lowering stress response through hypothalamus-pituitary-adrenal axis (using adaptogens).
~
7. Rebuild adrenals (adaptogens like ginseng, schisandra, nettles, burdock, ashwagandha, maca).
~
8. Balance of neurotransmitters (herbs like st. john’s wort, schisandra, ashwagandha, ginkgo, oatstraw, and siberian ginseng).
SAGE FLOWERS
This may feel like a lot to address, but as you can see many of the herbs overlap in these different categories. When I’m looking at support a specific system, this is how my mind organizes what I need to address. Some things may not be relevant in all situations, such as supporting deeper sleep if someone is sleeping really well already… or addressing nutrient deficiencies if they aren’t an issue, (which could be done through blood tests). If you can understand these basic elements of repairing the nervous system including the brain, you can apply them to a specific situation and person.
When I am recommending herbs I try to only give 2-3 remedies to take daily, with one of them being a water based infusion (tea or overnight infusion). It would not be hard to create a few blends that address most of these aspects of rebuilding the nervous system. I could create a tea infusion and a couple tincture blends or simples, introducing each one at a time before adding a new one.
My absolute favorite herbs to strengthen and support the nervous system are listed below. I try to include at last a few of them no matter what. As you can see they are all adaptogens except for oatstraw and skullcap, which I consider to be supreme nervous system restoratives. Other herbalists may add in a few others such as Bacopa, Ginkgo, Gotu kola, Codinopsis, Rhodiola, St. John’s Wort, Blue vervain, and Sage. There are certainly other amazing nervous system restoratives, these are just the ones I have seen to be the most effective over the years.
My favorite plants
to strengthen the nervous system ~
Oatstraw, Siberian Ginseng, Ashwagandha, Schisandra, Skullcap, Holy basil, Sage, Lavender, Evergreens
Audio ~ Caring for the Nervous System
SKULLCAP
Nourishing our Nerves
Addressing Nutrient Deficiencies with Vitamin Rich Plants
Vitamins and minerals play a crucial role in maintaining brain health and supporting the nervous system! For this reason our nourishing herbs are incredibly helpful for our brain and nervous system’s health. We can get our nutrients from multivitamins, from food, and from nourishing herbs. Our digestive system also needs to be functioning well for nutrients to be absorbed well. The right balance of nutrients is essential for neurotransmitter function in the brain, protecting neurons from damage, and allowing for communication between nerve cells. We can get our blood tested (and sometimes stool) to see what nutrients we might be lacking or not absorbing well. Below are key vitamins and minerals that contribute to brain and nervous system health, as well as the herbs we can use get them.
Nutrients for nervous system health ~
B Vitamins, Vitamin D, Magnesium, Calcium, Zinc, Iron, Copper, Selenium.
VITAMIN B1 (Thiamine) ~ Essential for converting carbohydrates into energy, which is critical for brain and nerve function. It also supports neurotransmitter synthesis, which helps regulate mood and cognition. Thiamine deficiency can lead to neurological problems, including memory loss and confusion. Sources: Nettles, Oatstraw, Dandelion, Chickweed. Whole grains, legumes, nuts, and seeds.
VITAMIN B6 (Pyridoxine) ~ Helps in the production of neurotransmitters like serotonin, dopamine, and gamma-aminobutyric acid (GABA), which are important for mood regulation and cognitive function. B6 also aids in reducing inflammation in the brain.
Sources: Nettles, Oatstraw, Dandelion, Chickweed. Poultry, fish, bananas, and potatoes.
VITAMIN B12 (Cobalamin) ~ Essential for maintaining myelin, the protective sheath around nerves that ensures efficient transmission of nerve impulses. It also plays a role in red blood cell formation, which delivers oxygen to the brain. A deficiency can lead to memory problems, mood disturbances, and neuropathy. Sources: Spirulina, Meat, dairy products, and fortified cereals.
FOLATE (Vitamin B9) ~ Involved in DNA synthesis and repair, which is essential for brain development and function. It also helps regulate homocysteine levels, a compound that, in excess, can lead to cognitive decline. Folate deficiency is associated with increased risk of depression and cognitive impairment.
Sources: Nettles, Oatstraw, Dandelion, Burdock, Chickweed. Leafy greens, legumes, and fortified grains.
VITAMIN D ~ Important for regulating mood and supporting overall brain health. Studies have shown that vitamin D deficiency is linked to cognitive decline and an increased risk of neurodegenerative diseases like Alzheimer’s. Sources: Nettles, Oatstraw, Dandelion, Chickweed. Sun exposure, fortified milk, and fatty fish like salmon.
VITAMIN E ~ A powerful antioxidant, vitamin E protects neurons from oxidative stress. It helps maintain the integrity of cell membranes and may slow cognitive decline associated with aging. Sources: Nettles, Oatstraw, Dandelion, Chickweed. Nuts, seeds, spinach, and broccoli.
MAGNESIUM ~ Involved in over 300 enzymatic reactions in the body, including nerve transmission and neuromuscular conduction. It also plays a role in the regulation of neurotransmitters like glutamate and GABA, helping to maintain healthy brain function and prevent conditions like anxiety and migraines. Sources: Nettles, Oatstraw, Dandelion, Burdock, Chickweed, Basil. Leafy greens, nuts, seeds, and whole grains.
ZINC ~ Crucial for synaptic plasticity, which is the ability of synapses to strengthen or weaken in response to activity, a process that underlies learning and memory. Zinc also plays a role in regulating neurotransmitter release and protecting against oxidative stress.
Sources: Nettles, Oatstraw, Dandelion, Alfalfa, Chickweed, Parsley, Ginger. Pumpkin seeds, sesame seeds, cashew, brazil nuts, hemp seeds, sunflower seeds, chia, flax, meat, shellfish, grains, beans (best soaked), nuts and seeds.
IRON ~ Necessary for oxygen transport to the brain and is involved in the synthesis of neurotransmitters like dopamine and serotonin. Low iron levels can lead to cognitive impairments, poor concentration, and mood changes.
Sources: Nettles, Oatstraw, Dandelion, Parsley, Chickweed, Thyme, Basil, Mint, Spirulina, Dill. Red meat, seeds and nuts like sesame seeds and hemp seeds, goji, beans, grains, seaweeds, leafy greens like spinach.
COPPER ~ Involved in the synthesis of neurotransmitters and the formation of myelin, which ensures the proper functioning of the nervous system. It also helps in the defense against oxidative damage in the brain.
Sources: Maca, Cacao, Shitake mushroom, Poppy seed, Turmeric, Basil, Mint, Cilantro, Black pepper, Fenugreek, Nutmeg, Fennel. Spirulina, sesame seeds, shellfish, nuts, seeds, and whole grains.
SELENIUM ~ Plays a vital role in reducing oxidative stress and inflammation in the brain. Adequate selenium levels are important for cognitive function and may help prevent neurodegenerative diseases. Selenium also plays an important role in reproduction and maintaining pregnancy, the function of the thyroid gland, production of DNA, and protecting the body from free radicals or infection Sources: Mustard seeds (highest), Ginger, Garlic, Onion, Parsley, Nettles. Brazil nuts, fish, oysters, eggs, and sunflower seeds.
DANDELION
NETTLES
CHICKWEED
SEAWEED
ALFALFA
Herbs to Nourish the Nerves
Nettle (Urtica dioica) ~
Contains significant amounts of vitamins B1 (thiamine), B2 (riboflavin), B6, B9 (folate), which are important for energy production, neurotransmitter synthesis, and nerve function. Stinging nettle also contains vitamins A, C, D, E, K, calcium, iron, magnesium, potassium, protein, beta-carotene, and chlorophyll.
~
Oatstraw (Avena sativa) ~
Rich in B vitamins, particularly thiamine (B1) and folate (B9), which help support cognitive function and mental clarity. Rich in Vitamin B, D, E, Magnesium, Calcium, and Iron. Oatstraw is also an amazing plant for reducing stress and anxiety.
~
Dandelion (Taraxacum officinalis) ~
Contains B vitamins, including B1 (thiamine), B6, and folate (B9). Also a rich source of vitamins A, C, D, iron, potassium, and zinc.
~
Chickweed (Stellaria media) ~
Stellaria species are rich in nutrients, including B vitamins (such as thiamine, riboflavin and niacin), magnesium, iron, calcium, zinc, vitamins C, A, and protein.
~
Burdock (Arctium lappa) ~
Contains B vitamins including folate (B9), magnesium, calcium, phosphorus, selenium, and potassium. It’s also high in vitamin C, choline, vitamin E, and K.
~
Alfalfa (Medicago sativa) ~
Rich source of B vitamins, calcium, iron, zinc, potassium, A, C, E, and K4. Alfalfa contains high levels of zinc, which is important for brain development and function, mood regulation, and neurotransmitter regulation.
Plantain (Plantago major) ~
High in vitamin A and C, calcium, magnesium, potassium, zinc, protien, and manganese.
Seaweeds ~
Rich in iron, magnesium, vitamin A, C, E, vitamin B9, iodine, vitamin K, fiber, DHA and EPA (omega fatty acids, potassium.
Red Raspberry ~
Excellent source of vitamin C, all B vitamins, iron, zinc, potassium, magnesium, and phosphorus.
~
Basil and Lemon balm ~
Both high in Magnesium, which is crucial for nerve function, relaxation, and mood regulation. Magnesium helps reduce stress, reduce tension, relieve anxiety, and supports sleep.
OATSTRAW
BURDOCK
Video ~ Nutrient Rich Plants for the Nervous System
ASHWAGANDHA
Regulating
The Autonomic Nervous System
Balancing Endocrine System Hormones
using adaptogens like ginseng, schisandra, and ashwagandha
as well as other endocrine tonics like chickweed, nettles, oatstraw
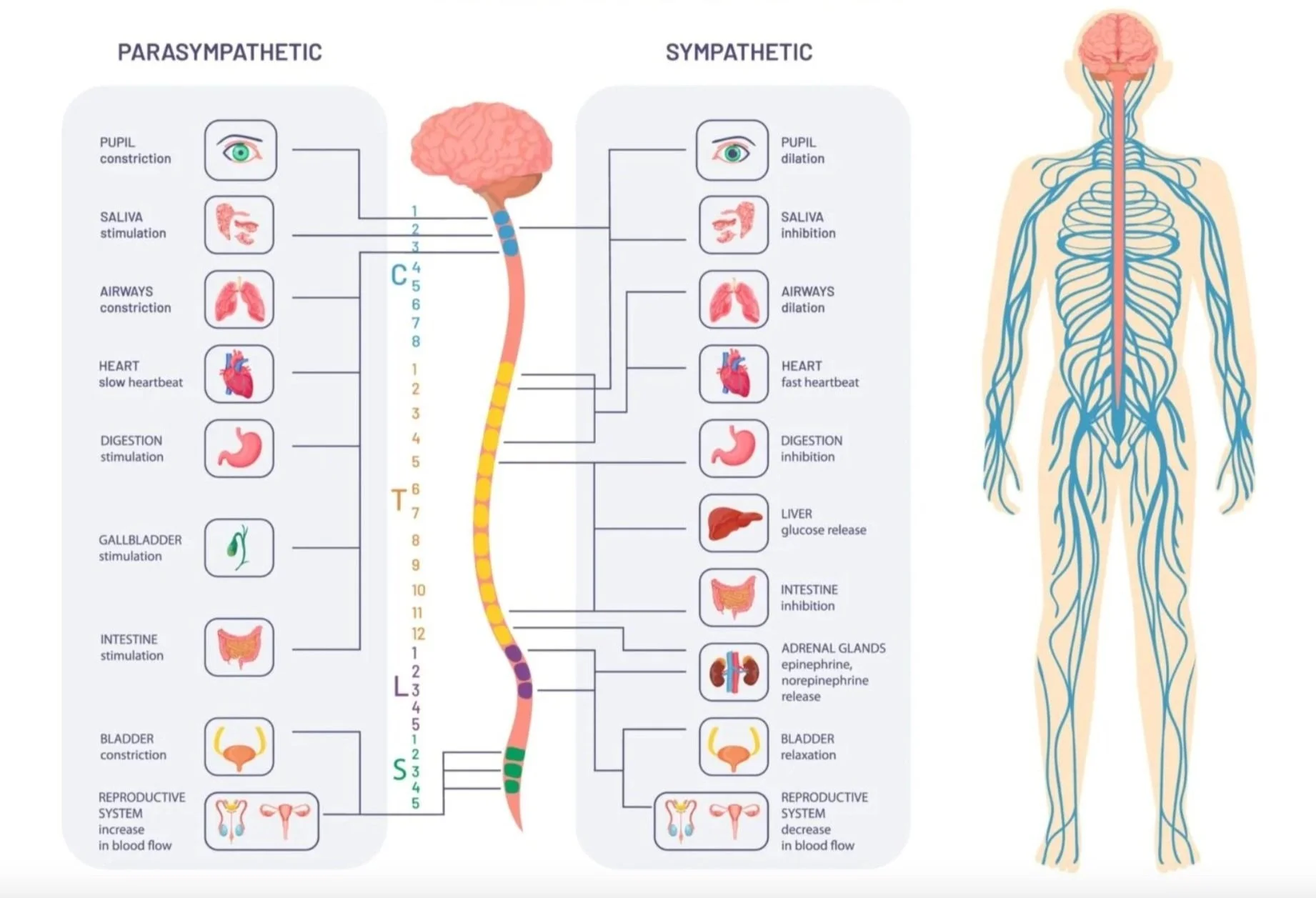
Our nervous system needs help regulating when we are under high levels of stress, anxiety, fear, or shock. As we covered in the first year, the involuntary (autonomic) nervous system is the primary mechanism in control of the fight-or-flight stress response. This means that we can’t control it, we can only impact it through different practices such as breathing and relaxation techniques, and of course herbs.
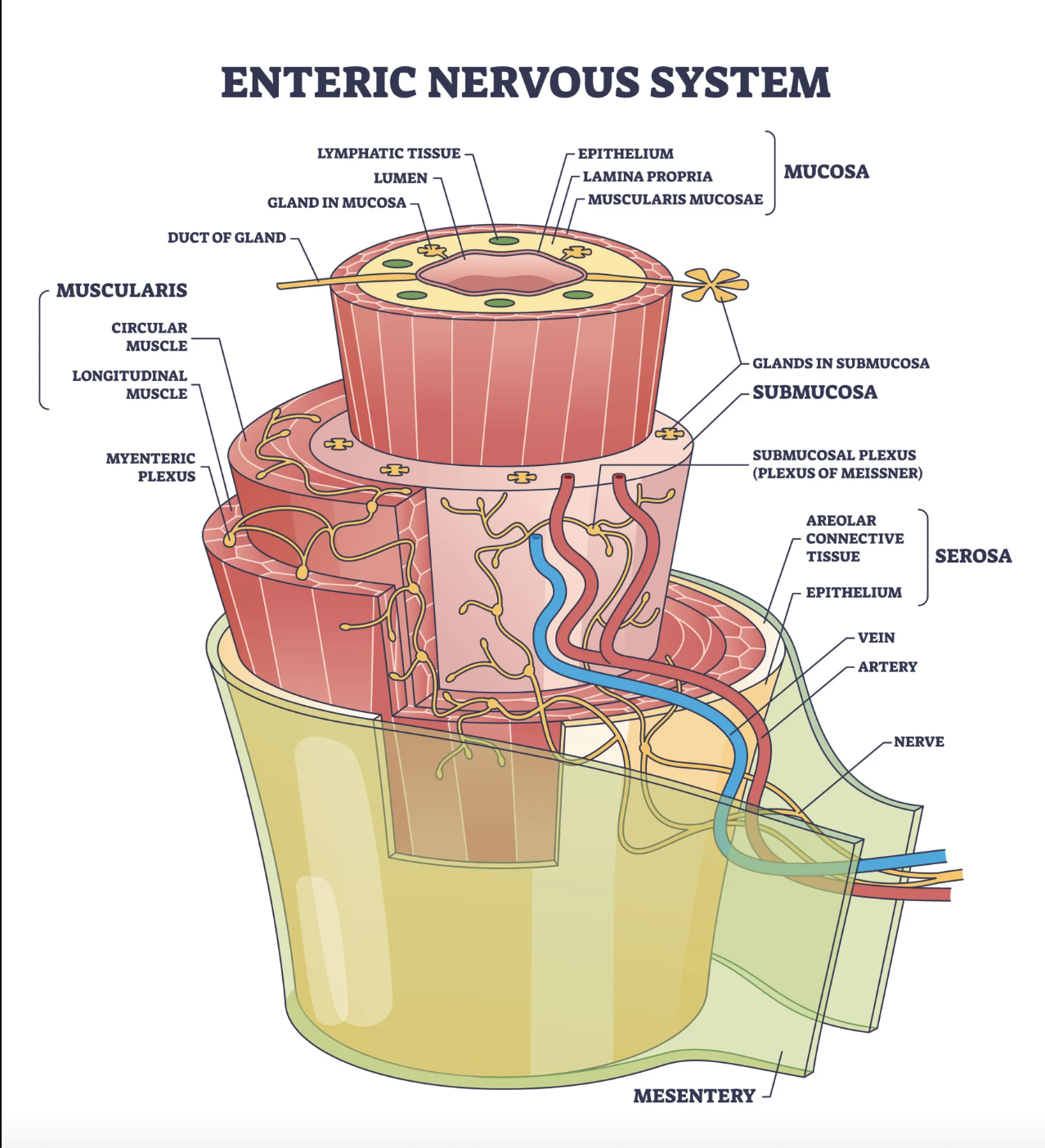
Our autonomic nervous system (ANS) controls our involuntary bodily functions, and stress response. It is regulated by the hypothalamus in the brain and your adrenal glands. The ANS transmits impulses from our brain and spinal cord to smooth organ muscles, cardiac muscle, and our endocrine glands. This includes regulating functions such as heart rate, digestion, respiration, and blood pressure.
The autonomic nervous system provides almost every organ with a double set of nerves - the sympathetic and parasympathetic. They work in tandem to each other to give us the state of relaxation and rest (parasympathetic) and excitement or action (sympathetic). Often one system activates a physiological response and the other inhibits it. The autonomic nervous system is responding continually to internal and external stimuli, which includes responding to our environment constantly. Adaptogens and calming herbs can be used to support stress management, promote relaxation, and maintain a healthy balance between the two systems, helping the body adapt to both stress and relaxation.
The parasympathetic nervous system (PNS) is the set of nerves that cause relaxation, which is responsible for the "rest and digest" functions of the body. It conserves energy instead of burning energy, and stimulates the body to focus on healing. The PNS helps the body relax after stress, lowers blood pressure and heart rate, as well as regulates normal body functions during periods of calm. The left and right vagal nerves contain 75% of your parasympathetic nervous system’s nerve fibers, which means your vagal nerves are responsible for most of your body’s relaxation. These fibers send information between your brain, heart, and digestive system, helping us to go into the “rest and digest” state.
Relaxants
Inviting Peace & Relaxation
PASSIONFLOWER
Herbs that activate the parasympathetic nervous system are nervines and calming adaptogens. They can also help us to slowly release from the frozen state, calming any panic residing underneath. We have covered the nervines extensively, but I want to talk about dosing that will be the best during intense moments of stress. I recommend taking 3-4 droppers full in water every couple hours until relief is eventually felt.
Ashwagandha (Withania somnifera) ~ One of my favorite adaptogens and nervines, amazing for reducing stress and anxiety, Ashwagandha promotes parasympathetic activity by helping the body relax and recover from stress. The root tastes sweet and earthy, and is safe to take daily. It is very balancing to hormones, anti-inflammatory, antidepressent, and helpful for deeper sleep. In times of high stress it will lower cortisol levels and calm an overactive stress response. Ashwagandha is also known to help with building healthy muscles and increasing energy or endurance. I love the grounding and stabilizing feel of ashwagandha. Take 2-3 droppers full of tincture in a glass of water 2x a day.
Skullcap (Scutellaria lateriflora) ~ Skullcap is one of the absolute best nervines for longer term constant use. It’s in the mint family and can be taken daily (often many times a day) to reduce anxiety or overwhelm. It’s especially helpful someone’s stress is connected to overworking, addictions, trauma, or chronic stress. It can help improve sleep, relax the muscles in the body, and quiet the mind. I love the taste and feel of skullcap because it is so opening to the lungs and helpful for releasing all kinds of emotional tension. Take 2-4 droppers full of tincture in a glass of water 2-3x a day.
Lemon Balm (Melissa officinalis) ~ Lemon balm helps reduce anxiety and promotes relaxation by enhancing parasympathetic nervous system activity. It’s especially nice to drink as a tea, soothing to digestion, uplifting when we have the blues, and helpful for sleep. Lemon balm is gentle and relaxing to tension we hold in our body and bellies. Wonderful for kids, especially as a tea or sweet glycerite. Drink the tea or take 2-4 droppers full of tincture in a glass of water 2-3x a day.
Peach (Prunus persica) ~ Peach is fast becoming my favorite nervous system relaxant. It’s related to rose, hawthorn, and cherry, with a sweet cooling energy. I love that it’s a heart tonic, anti-inflammatory for the whole body including the musculoskeletal system, pain relieving, antidepressant, and deeply relaxing to anxiety.
Linden (Tilia cordata) ~ Linden is sweet and soothing to the nerves, enhancing the parasympathetic response and helping us to feel safe. This is the tea I often give students when they first come to class. It’s sweet tasting, demulcent, and a wonderful nerve tonic to release anxiety or fears. I find the smell of the flowers intoxicating and love these trees deeply. Linden is also a great heart tonic as well as soothing to the digestive system. I prefer linden as a tea or sweet in a glycerite.
Stimulants
Excitement & Activity
RHODIOLA
The sympathetic nervous system helps us to have energy and wake up when we need to! This system is responsible for enabling quick responses to stress or danger and increases energy during times of excitement or perceived threat. It promotes activity and action in the body, as well as the "fight or flight" response. This is caused by a release of adrenaline and other stress hormones such as cortisol from the adrenals, signaled by the hypothalamus in the brain.
The sympathetic nervous system is part of our involuntary nervous responses that prepare the body for action, causing alertness and arousal. It also causes burning of energy and over time can make us feel depleted and tired. The sympathetic nervous system increases the release of sugar from the liver into the blood so we have higher blood sugar for our cells to have the fuel they need. During the stress response blood flow diverts away from the gastro-intestinal tract and skin from vasoconstriction. Blood flow is enhanced to the skeletal muscles, lungs, heart, and brain, by as much as 1200% in the case of skeletal muscles. This allows us to run from the bear (in theory) during the stress of a possible threat or attack.
The bronchioles (air vessels) in our lungs also dilate from the circulating epinephrine, which increases the oxygen our body can receive for the energy we need. It provides vasodilation for the coronary vessels of the heart, allowing more blood flow to the heart and increases our heart rate. Our pupils dilate, which allows more light to enter the eye and provides further reaching vision. Our digestive system slows down by constricting all the intestinal sphincters and the urinary sphincter. Since we have extra blood flowing to the brain, we often feel more alert and focused. We feel energized because our cells are receiving more fuel, and adrenaline is pumping through our bloodstream from the adrenals. This active state allows us to be able to do all of the activities we love, as well as work hard when we want to! Most of us drink coffee and tea or some other stimulates to activate the sympathetic nervous system. Over time this is certainly exhausting to our system without enough rest.
When we stay in the sympathetic state for too long of a period, it exhausts our endocrine and nervous systems. The resulting symptoms are varied and many… chronic stress, fatigue, anxiety, weight gain (from too much cortisol in the blood stream), frazzled nerves, physical weakness, exhaustion, unclear thinking, insomnia, high blood pressure, damage to the heart and blood vessels, depleted adrenals, eventual low cortisol and often depression. Without enough cortisol, which is a natural anti-inflammatory, we have have chronic inflammation and an immune system that can be overactive leading to allergies or autoimmune issues.
Herbs that stimulate and activate the sympathetic nervous system ~
TEA
Ginseng (Panax ginseng) ~ Ginseng is an adaptogen that stimulates the sympathetic nervous system, and for some people can cause feelings of being too gittery if it is taken at too high a dose. Ginseng increases energy, improves focus, and enhances physical endurance during times of stress or fatigue. It is also hormone balancing, immune strengthening, and a helpful anti-depressant.
Rhodiola (Rhodiola rosea) ~ Rhodiola can be activating and energizing while still helping to balance the body's stress response and prevent excessive over activation. Rhodiola boosts energy and increases mental alertness, while also helping to calm when stress levels are high. Similar to ginseng we do not want too high of a dose or we can feel overstimulated. Rhodiola is also a heart tonic, which can feel especially soothing and sweet. I find it to taste like an earthy rose tea and it’s really helpful when we need an adaptogen that has really lovey energy.
Coffee & Black or Green Tea ~ Coffee and tea are of course the most preferred stimulants around the world, which are both activating to the sympathetic nervous systems and help us have both focus and energy. Both are strongly antioxidant, and coffee is a useful bitter for the digestive system. However we do want to be careful to not over stimulate the adrenals with excessive coffee drinking. Green tea is much lower in caffeine and highly antioxidant, causing it to be a wonderful tonic for the brain and heart.
Video ~ Plants to Energize & Stimulate
Feeling Frozen, Numb, and Disconnected
The Freeze State
We all have moments of feeling shut down, numb, and frozen. It tends to happen when there is mental and emotional overwhelm during a very stressful period of time or after traumatic experiences. When the sympathetic nervous system is in high ‘fight or flight’ activity/stress response, often the parasympathetic steps in to “cap” it and control it. As we talked about in the first year module, this results in a “frozen” state that often has feelings of disassociation and high levels of fight or flight hidden underneath. As this frozen state releases, the fight or flight stress response is experienced.
Many of us know the freeze state as a strange feeling of calm we may experience during emergency or high stress situations. Underneath the outer calm is buried a deeper layer of emotions, anxiety, and fear that will eventually have to release. As we slowly come out of a frozen state we have to be careful of the emotions, anger (fighting), or desire to run that could release underneath. You can take daily, and sometimes hourly, nervine herbs to bring down the stress residing underneath of a frozen state. Often it takes a certain level of safety for the panicked frozen state to release, but we have to be careful we don’t harm those around us when the pain releases underneath. Safe spaces to cry, scream, yell, shake, and move our bodies can help us release the emotions we need to let out of our bodies.
Audio ~ Herbs for Managing the Freeze State
NETTLE SEED
Regulating Cortisol
& Building Adrenals
Reducing Stress Response & Stress Hormones
with adaptogens like ginseng, schisandra, nettles, rhodiola, holy basil, licorice, eleuthero, ashwagandha, reishi, maca
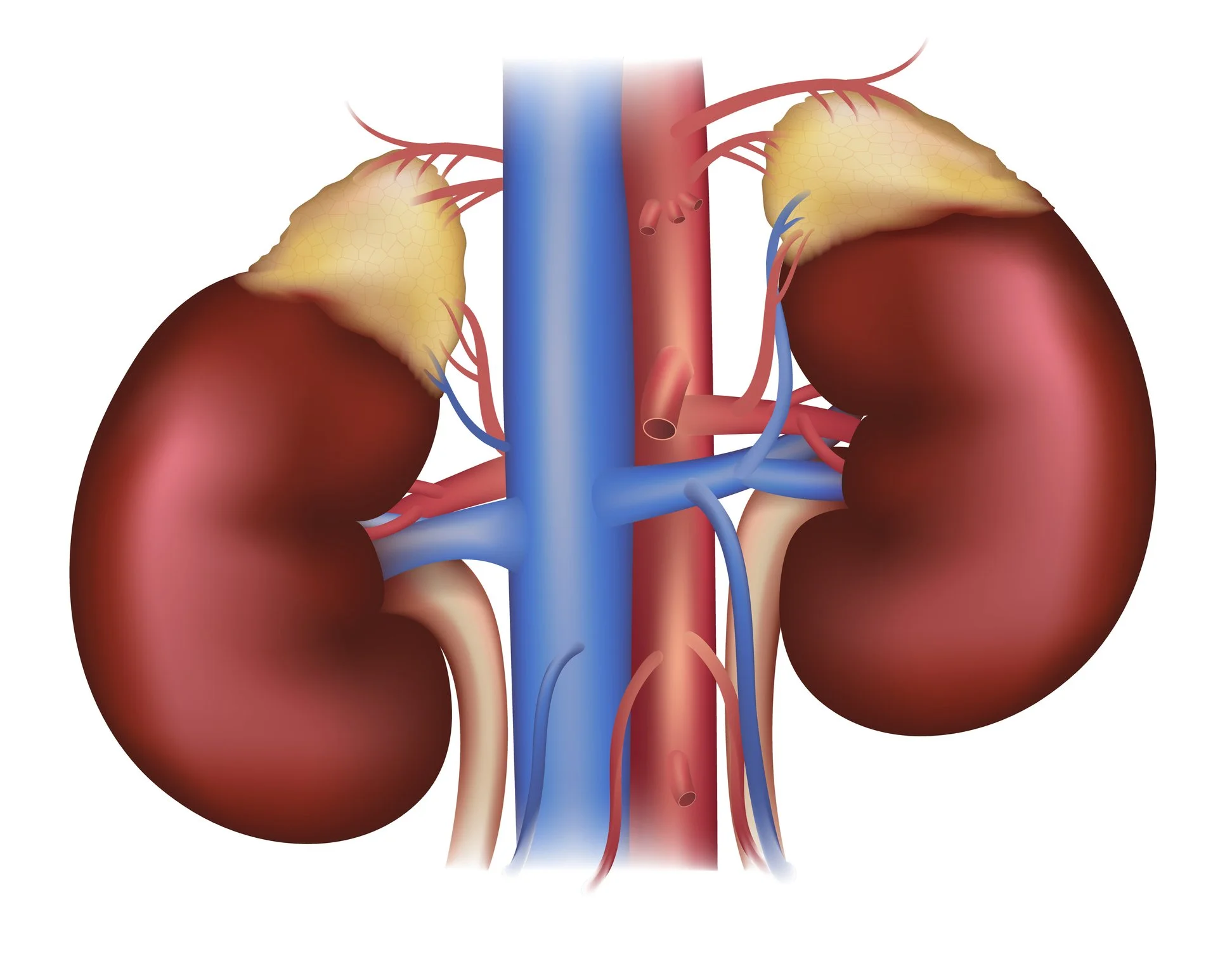
We all know the importance of our adrenals to give us energy. They are the endocrine organs responsible for helping us wake in the morning and being active during the day! We love coffee and black tea not just for the taste, but to give us energy throughout the day to do things we want to do. The adrenals also help regulate different body functions when we are active and expending energy, as well as during moments of stress or excitement. The adrenals produce very important hormones such as cortisol, aldosterone, and androgens like testosterone. We will look at cortisol first, and then the other hormones we receive from our adrenals and the effects they have.
Cortisol is often called the “stress hormone” because it helps the body respond to activity and stress by increasing blood sugar to give your body fuel for energy. Cortisol helps in regulating metabolism by influencing how the body processes carbohydrates, proteins, and fats so the body has energy when its needed. Cortisol also has potent anti-inflammatory properties, helping to control the body’s immune responses. Cortisol suppresses inflammation in the body, and represses the immune system from overreacting.
Cortisol is a natural anti-inflammatory that prevents chronic inflammation, allergic reactions, and auto-immune diseases. When there is too little cortisol this can result in an overactive immune system. This means there is adrenal insufficiency and we have to build up the health of the adrenals to get cortisol levels back up to normal.
Low Cortisol
and Cortisol Resistence
There are two reasons we may not have the cortisol we need - 1. when the adrenals are not producing enough because we have adrenal depletion. 2. When high levels of cortisol from chronic stress causes the body to become resistant to cortisol’s effects, similar to how the body can become resistant to insulin in diabetes. This can result in an overreactive immune system causing increased allergic reactions, auto-immune illnesses, and chronic inflammation.
Certain herbs particularly adaptogens, help the body cope with stress and can improve cortisol sensitivity such as astragalus, rhodiola, ginseng, reishi, ashwagandha, holy basil, maca, nettles, and burdock. Chronic inflammation contributes to cortisol resistance, so reducing inflammation in the body can help restore cortisol sensitivity. Increasing water intake, omega-3-rich foods (like fish) can reduce inflammation, as well as anti-inflammatory herbs such as turmeric, ginger, burdock, licorice, marshmallow root, cat’s claw, japanese knotwood, evergreens, salicylic acid contianing herbs like willow, birch, cottonwood, or magnolia.
REISHI
Reducing High Cortisol
When there is too much cortisol as a result of chronic stress, it effects the body in many ways. Besides leading to cortisol resistance, high cortisol can cause fatigue, high blood pressure, headaches, irritability, difficulty concentrating, mood swings, anxiety, and depression due to the hormone's impact on the brain. It can also cause weight gain, acne, thinning skin and hair, easy bruising, flushed face, slowed healing of wounds, osteoporosis, and muscle weakness. Prolonged elevated cortisol can suppress the immune system making someone more susceptible to infections, as well as causing insulin resistance, which can lead to type 2 diabetes.
There are many ways to reduce high cortisol levels. Since fluctuations in blood sugar levels can trigger cortisol spikes, eating regular meals with a good balance of protein, healthy fats, and fiber helps stabilize blood sugar and reduce the need for cortisol to intervene in blood sugar regulation.
Not getting enough sleep can also lead to elevated cortisol levels and worsen cortisol resistance. Improving sleep quality is crucial for restoring the body's normal cortisol rhythms. Regular moderate exercise can also lower cortisol levels and improve the body's sensitivity to cortisol, but it’s important to avoid over-exercising, as intense or prolonged exercise can increase cortisol production. Chronic stress and overwork can contribute to high cortisol levels, which can cause cortisol sensitivity so it’s important to make time for relaxation and self-care. Engaging in activities that bring joy and relaxation, such as spending time in nature, socializing with loved ones, or pursuing hobbies.
Adaptogens such as Ashwagandha, Rhodiola Rosea, Holy Basil, Panax Ginseng, Licorice Root, Schisandra, Reishi, Maca Root, and Eleuthero are effective natural remedies for reducing cortisol resistance. By regulating cortisol production, supporting adrenal health, and improving the body’s stress response, these herbs help restore balance in the HPA axis and reduce the risk of long-term cortisol-related health issues.
Cortisol & Allergies
High stress levels often cause an increase of allergies and allergic reactions. Chronic stress and high cortisol can also lead to imbalances in immune function, causing certain immune cells, like mast cells, to become more reactive. Mast cells are responsible for releasing histamine when they detect an allergen, and if they become overactive, even minor exposures to allergens can trigger stronger allergic responses. This means high stress can cause more hay fever, asthma, or skin conditions such as eczema.
High cortisol levels can also weaken the protective barriers of the skin, gut, and respiratory tract, which normally help prevent allergens and pathogens from entering the body. When these barriers are compromised, the immune system may encounter more allergens, increasing the frequency and severity of allergic reactions.
Herbs for Adrenal Health
ADRENAL GLANDS & KIDNEYS
Nettles (Urtica dioica) ~ Nettle seed is an adrenal tonic and as an adaptogen are able to modulate our stress response. A tincture of the seeds are good for helping with adrenal burnout and rebuilding after (or during) chronic stress. This can increase the production of adrenalin and cortisol as the adrenals slowly return to proper functioning. Nettle seeds can help with fatigue and boost energy levels over time, increase st mental clarity, and stamina, making them particularly helpful in cases of adrenal fatigue where the body’s energy reserves are depleted. Studies showed that nettle seed can regulate the body's stress response by balancing the production of cortisol and other adrenal hormones. Nettle seeds are also rich in nutrients such as magnesium, zinc, iron, calcium, and essential fatty acids, all of which are crucial for adrenal health. The seeds are also a powerful kidney tonic, which helps improve adrenal function as well. Dose ~ 15 -30 drops to start in water. Can go up to 2 droppers full in water 3x a day. Nettles seed will be overstimulating for some people.
~
Ashwagandha (Withania somnifera) is an amazing adaptogen to strengthen the adrenals and nervous system. It is a great nervine to calm stress and anxiety, improve sleep, regulate neurotransmitters, and ease depression. The root and leaves can balance cortisol levels and support adrenal recovery during chronic stress or burnout. Ashwagandha as all of our adaptogens, helps regulate stress through modulating the hypothalamic-pituitary-adrenal (HPA) axis, the body’s central stress response system. By enhancing the body's ability to cope with physical and emotional stress, it can help restore cortisol sensitivity and alleviate the symptoms of cortisol resistance. I am in love with the calming, earthy, strengthening feeling of ashwagandha.
Dose ~ 2-4 droppers full of the tincture in water two or three times a day. For the tea brew 1-2 tsp of the root powder in 1 quart hot water steeped 30 minutes.
Rhodiola (Rhodiola rosea) ~ Rhodiola is a sedum that has a rose smelling root growing in cold mountain elevations in Europe, Asia, and North America. The tea tastes a bit like rose and dirt combined, both grounding and sweet. It is an adaptogen that has been used for thousands of years, enhancing mental or physical stamina and endurance, as well as recovering from burnout and exhaustion. Rhodiola helps the body adapt to stress, reduces fatigue, and strengthens the adrenals. It is particularly helpful for people dealing with exhaustion from prolonged stress. Rhodiola balances the stress response, lowers stress hormones, reduces cortisol resistance, and regulates neurotransmitters. It can be a great anti-depressant, increase mental focus, and enhance dopamine and serotonin activity. Dose ~ 1-3 droppers full of the tincture in water two or three times a day. For the tea steep 1-2 tsp of the root in 1 quart of hot water for 30 minutes.
TULSI
Holy Basil (Ocimum sanctum) ~ Tulsi is another amazing adaptogen we’ve explored already, but this one is a fragrant and heavenly minty basil used in Asia for thousands of years. It helps reduce stress and anxiety, strengthen the adrenal glands, balance cortisol levels, and reduce cortisol resistance. It’s also a tonic for the brain, increases mental clarity and regulates neurotransmitters. Tulsi helps regulate the body's response to chronic stress, lowers anxiety, and reduces inflammation and oxidative stress. Dose ~ 2-4 droppers full of the tincture in water two or three times a day. For the tea brew 2-3 tsp added to 1 quart hot water and steeped 30 minutes.
~
Schisandra chinensis is one of our most beloved adaptogens, with sour berries that give us energy like no other plant I know without caffeine. This adaptogen regulates the body’s stress response, reduces cortisol resistance, and strengthens the adrenal glands. Schisandra helps restore balance to the HPA axis, improves tolerance to stress, and regulates cortisol levels. Schisandra is also a brain tonic, neuroprotective, anti-inflammatory, fluid cleansing, kidney and liver strengthening, as well as hormone balancing. We love it’s energizing feel and sour zing! Dose ~ 2-4 droppers full of the tincture in water two or three times a day. For the tea simmer 3 tsp berries to 1 quart hot water for 20 minutes.
Eleuthero (Eleutherococcus senticosus) ~ (often referred to as Siberian Ginseng) ~ My three favorite adaptogens for the nervous system are ashwagandha, schisandra, and eleuthero. Siberian ginseng is a grounding, earthy, and calming adaptogen known for helping us have sustained energy, improved brain function, and reduced fatigue. Like the other adaptogens it lowers our stress response and helps balance cortisol production. Eleuthero strengthens the adrenals, helps the body recover after stressful events, and restores hormonal balance. It can increase energy levels and mental focus without overstimulating the body. Eleuthero is especially good for anyone with chronic fatigue and physical exhaustion. Athletes have used it for hundreds of years for endurance and mental focus in Russia, Siberia, and parts of Asia.
PANAX GINSENG
Panax ginseng is a well-known adaptogen that supports overall energy and mental clarity, while also helping the body balance cortisol levels. Ginseng enhances the body's stress response and reduces the release of excessive cortisol during stressful situations. It has been found to lower chronic stress-induced cortisol levels and improve the body's sensitivity to cortisol, helping those with cortisol resistance regain proper hormonal balance. In addition to improving physical resilience, Ginseng supports cognitive function and mental stamina, helping individuals feel more balanced and focused even during stress.
Licorice Root (Glycyrrhiza glabra) ~ Licorice root is an adaptogen especially helpful for adrenal burnout, low cortisol levels, or cortisol resistance, because it slows the break down of cortisol in the body. It is also strengthening to the adrenals, increases energy levels, and boosts the immune system (as all adaptogens do). Licorice also reduces inflammation throughout the body, especially in the respiratory and digestive tracts. It should be used with caution in people with high blood pressure since it has been known to increase BP especially in people who have edema.
Maca Root (Lepidium meyenii) is a sweet tasting adaptogen that’s also cooked and eaten as a food in the Andes. The bulbous root that looks like a beet has been traditionally used to balance hormones, increase energy and endurance. Like the other adaptogens, Maca helps regulate the body’s response to stress, increases resilience after stress, strengthens the adrenal glands, and balances cortisol levels. Maca feels very nourishing, grounding, and demulcent, wonderful made into a tea and added to smoothies or cereals. It can reduce fatigue and give long lasting energy.
Herbs for the kidneys (also supporting adrenals) ~
Dandelion, Burdock, Nettles, Astragalus, Parsley, Milk thistle, Licorice,
Turmeric, Goldenrod,Cranberries,
Video ~ Plants for Adrenal Health
ST JOHNS WORT
Balance of Neurotransmitters
with herbs like st. john’s wort, schisandra, ashwagandha, ginkgo, oatstraw, and siberian ginseng
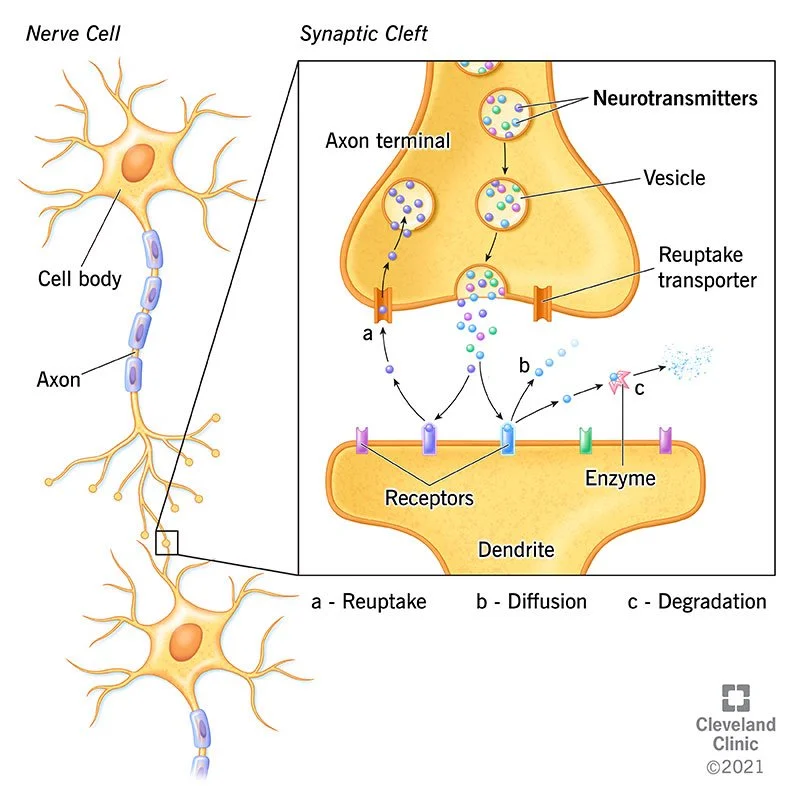
Many issues of brain function and nervous system health are connected to imbalances in neurotransmitters, which are the chemicals our nerves use to send messages throughout the brain and body. All of us have an understanding of neurotransmitters affecting our mood and brain function to some degree. It’s important to recognize that emotions and experiences we have can alter these chemicals in our brain. When we have a lot of stressful or emotional experiences especially as a child, our brain and neural chemistry is impacted. There is a lot we can do to help someone return to a healthy chemical balance, understanding that there is not one normal… just many variations of the human brain and experience.
Neurotransmitters like serotonin, dopamine, GABA, and acetylcholine in our brain and nervous system regulate a lot of our body’s processes including mood, sleep, memory, stress, and motor functions. Balancing and supporting healthy neurotransmitter levels is important for not only mental health but physical health as well. Plants can effect neurotransmitters in many different ways, which we will explore in depth. I hope this thorough investigation of how plants effect our brain chemistry can help you understand more of how we can use them to help support others mental and emotional health. Be careful with combining herbs and Western medications that also effect neurotransmitters, since there can be interactions. I recommend using WebMD to look up herb-drug interactions when needed!
In the diagram to the right you can see neurotransmitters jumping from one nerve cell to the next. One nerve cell releases a chemical neurotransmitter and passes it the next nerve cell. The neurotransmitter binds to a receptor on the surface of the receiving cell, sending its chemical message. There are over 100 different neurotransmitters identified, though there are possibly 100-200 more unknown. Each neuron produces and releases only one or a few types of neurotransmitters, but can carry receptors on its surface for several. There are a few problems that can cause poor neurotransmitter transmition between nerve cells. Reuptake is when neurotransmitters are reabsorbed into the nerve cell instead of being sent to the next cell. Enzymatic degradation is when enzymes break down the neurotransmitters before the next nerve cell receives them, and diffusion is when neurotransmitters migrate away from the receiving nerve cell.
When certain neurotransmitters are either deficient or in excess we can see significant disruptions in brain function as well as the development of illnesses. For example low levels of serotonin can cause depression. Dopamine imbalances can cause schizophrenia, Parkinson’s disease, and contribute to ADHD. Anxiety disorders have been found to be connected to GABA (gamma-aminobutyric acid) dysfunction. GABA is a neurotransmitter that calms brain activity, and when GABA levels are low people can have heightened anxiety such as panic attacks.
Many people with ADHD and PTSD also experience norepinephrine imbalances. Inattention, restlessness, and hyperactivity disorder (ADHD) are symptoms of abnormal norepinephrine levels. Anxiety, tension, and post-traumatic stress disorder are all associated with abnormal norepinephrine levels. Memory and learning are influenced by the neurotransmitters glutamate and acetylcholine. The neurotransmitters melatonin and gamma-aminobutyric acid (GABA) have a role in the regulation of sleep cycles. Depression, anxiety, insomnia, schizophrenia, and Parkinson's disease are just some of the physiological processes that may go haywire when neurotransmitters aren't working as they should. The two most well-known classes of neurotransmitters are inhibitory and excitatory. Excitatory neurotransmitters encourage neurons to fire more often, whereas inhibitory neurotransmitters decrease neuronal activity.
Bipolar disorder is associated with changes in mood and is believed to be influenced by imbalances in neurotransmitters such as serotonin, dopamine, and norepinephrine. Low levels of the neurotransmitters dopamine and norepinephrine contribute to lethargy, depression, and lack of drive during the depressed phase, whereas high levels of these neurotransmitters can cause increased energy, impulsivity, and euphoria during the manic phase. Moreover, serotonin and dopamine pathway dysregulation is linked to OCD, which in turn contributes to the repetitive pattern of intrusive thoughts and actions. Acetylcholine is especially impacted in neurodegenerative disorders such as Alzheimer's disease, which also involve failure of other neurotransmitters. One reason why people with Alzheimer's experience memory loss and cognitive impairment is because of the degeneration of neurons that produce acetylcholine.
VALERIAN ROOT HARVEST AT GAIA
Many herbs we’ll discuss have been shown in studies to modulate neurotransmitter levels, balancing brain chemistry naturally. I’m including herbs that have been shown in studies to effect specific neurotransmitters, either by enhancing their production, regulating neurotransmitter receptors, or inhibiting the enzymes that break neurotransmitters down. I find these plants to be very effective for all kinds of brain and nervous system support through experiencing them over the last few decades in action… But it’s great to see the science back up what we see works! Please note these herbs should be used consistently and over a period of at least 1-3 months to see the best results.
There are many herbs recognized to help to maintain neurotransmitter balance.
St. John's Wort increases serotonin, dopamine, and norepinephrine levels in the brain, which improves mood and reduces depression. It’s shown in studies to be as effective as SSRIs for mild to moderate depression with fewer side effects. Rhodiola balances serotonin, dopamine, and norepinephrine, increasing brain function and our stress tolerance. Ginkgo biloba affects acetylcholine and dopamine, neurotransmitters effecting brain funtion, memory, attention, and learning. It’s been used for thousands of years to address cognitive decline and neurodegenerative diseases including Alzheimer's disease.
Raising GABA levels helps us relax and lessens neuronal overactivity since GABA is the main inhibitory neurotransmitter helping to lower brain excitability and encourage relaxation. Since passionflower raises GABA levels in the brain it’s often used for anxiety and sleeplessness. Valerian stops the breakdown of GABA breakdown, increasing levels in the brain. Skullcap also lowers anxiety by increaing GABA activity in the brain and reduces neural excitability. Ashwagandha, another adaptogen, modulates GABA and serotonin to reduce stress and anxiety. It lowers cortisol and balances excitatory and inhibitory neurotransmitters to support the nervous system. Clinical studies demonstrate ashwagandha improves anxiety, stress, and cognition. These are just some of the examples of herbs effecting our neurotransmitters.
Holistic Ways to
Balance Neurotransmitters
From genes to environmental effects, a number of things can affect the synthesis, release, and action of neurotransmitters. For the brain to create neurotransmitters, certain nutrients are needed, which we explored in the first part of this module. Deficiencies in amino acids or vitamins and minerals like B vitamins, magnesium, and zinc can cause the imbalance of neurotransmitter levels. The amino acid tryptophan in bananas, nuts, seeds, and turkey is a precursor of serotonin. Tyrosine found in chicken, soy, and dairy products is a precursor of dopamine and norepinephrine. Vitamin B6 is essential for GABA and serotonin to be produced. Eating a lot of processed foods and not getting our essential nutrients can lead to depression and cognitive decline due to the resulting neurotransmitter imbalances. Foods high in Omega-3 fatty acids like salmon and other seafood increase the health of nerves and neurotransmitters inproving brain function.
What Affects Neurotransmitter Levels?
Many other therapies besides herbs help to balance neurotransmitters. Physical activity increases the production of endorphins, dopamine, and serotonin, which improves mood, reduces stress, and enhances cognitive function. Regular exercise has been shown to alleviate symptoms of depression and anxiety. Other practices like mindfulness meditation can also increase serotonin and GABA levels while decreasing cortisol, the body’s primary stress hormone.
Prolonged stress creates neurotransmitter imbalances, especially involving norepinephrine, serotonin, and dopamine. Excessive amounts of stress raise cortisol production, which can disrupt neurotransmitter activity. Long-term stress lowers serotonin and dopamine levels, which causes anxiety, sadness, and burnout symptoms. People who experience ongoing stress have changed neurotransmitter levels, which can result in mood changes, emotional swings, and poor brain function.
Neurotransmitter levels and activity can be greatly impacted by alcohol, nicotine, and some prescription medications. Although alcohol increases GABA activity, which promotes relaxation, long-term usage can lower serotonin and dopamine levels, which can make depression worse. Western medications used for depression and anxiety can cause lowered production of neurotransmitters in the brain when used long term, creating dependance. Selective serotonin reuptake inhibitors (SSRIs) raise serotonin levels by preventing serotonin from being reabsorbed in the brain and reducing depression. Long-term drug use can change how neurotransmitters are naturally produced in the brain, which can cause dependence and cognitive deterioration.
Physical activity increases the release of endorphins, serotonin, and dopamine, which improves mood, reduces anxiety, and enhances brain function. Regular exercise has been shown to alleviate symptoms of depression and anxiety by increasing the availability of neurotransmitters that promote mental well-being.
Sleep is really important for the balance of neurotransmitters - especially serotonin, dopamine, and norepinephrine. Sleep deprivation lowers the production of serotonin and dopamine, which results in mood swings and cognitive decline. Lack of sleep can drastically change neurotransmitter levels, which can lead to symptoms of anxiety, depression, and impaired brain function.
Neurotransmitter function and general brain health can be greatly affected by exposure to environmental pollutants such pesticides, heavy metals, and air pollution. Lead and mercury are two examples of toxins that can harm neurons and throw off the glutamate and GABA neurotransmitter equilibrium. Changes in neurotransmitter activity, neurodegenerative disorders, and cognitive impairment are linked often to prolonged exposure to environmental pollutants.
Neurotransmitter function is also significantly influenced by genetics. Single nucleotide polymorphisms (SNPs) are genetic changes that can impact neurotransmitter synthesis, release, and degradation. Dopamine breakdown in the brain is impacted by variations in the COMT gene, which can impact mood, cognition, and vulnerability to mental health disorders. Higher rates of anxiety and depression are linked to genetic predispositions to lower serotonin or dopamine levels.
Neurotransmitter
Imbalances
Here is a short summary of some herbal approaches to various neurotransmitter imbalances. I go into further detail as we discuss each neurotransmitter and herbs we can use to support its healthy balance in the brain. Please remember that we have to address the causes of the neurotransmitter imbalance if possible, and use holistic therapies besides herbs… such as diet, sleep, exercise, stress reduction and relaxation practices. Understand that herbs will interact with Western medications, so always check on Web MD any drug interactions, and make sure someone is also working with a doctor to have medical supervision when using herbs and meds together.
Depression
Depression is often linked to low levels of serotonin, dopamine, and norepinephrine. Antidepressants such as SSRIs are used to increase serotonin levels, but there are many holistic alternatives such as herbs, exercise, and a healthy diet to support neurotransmitter balance. All herbs that increase serotonin, dopamine, norepinephrine, and GABA (lowering anxiety and stress) can reduce depression. As you read through this module you’ll see all of the herbs we discuss can be effective treatments for depression caused by neurotransmitter imbalances.
Herbal therapies ~ St. John’s Wort, Rhodiola, Panax ginseng, Ginkgo, Ashwagandha, Lemon balm, Schisandra, Holy basil, Gotu kola, and most adaptogens.
Fibromyalgia & Chronic Pain
Our body's pain pathways can get very out of whack. Neurotransmitters like serotonin, norepinephrine, and GABA play a big role in this, especially when it comes to chronic pain syndromes like fibromyalgia. When the body struggles to block pain signals due to low neurotransmitter levels, it can lead to feeling pain more intensely. Chronic pain disorders might be linked to a deficiency in GABA. This neurotransmitter reduces feelings of anxiety and stress as well as helping to keep pain sensations in check. Medications like pregabalin (Lyrica) can help with pain management by modulating GABA. Many people also manage fibromyalgia or chronic pain with medications such as SNRIs that boost serotonin and norepinephrine levels. So many amazing nervine herbs can boost GABA and help with pain managemen. Passionflower, Skullcap, Blue Lotus, Valerian, Blue Vervain, and Lemon Balm are just a few. When pain is mostly due to inflammation, we turn to our best anti-inflammatory herbs while also tackling the root causes of any tissue damage.
Herbal therapies ~ Skullcap, Passionflower, Oatstraw, Ashwagandha, California Poppy, Lavender, Valerian, St. John’s Wort, Rhodiola, Oatstraw, Lemon balm, Blue vervain, Peach, Catnip, Gotu kola, Black cohosh, Ginkgo
Anti-inflammatories ~ Turmeric, Ginger, Cat’s claw, Licorice, Willow, Cayenne, Meadowsweet, Peach, Birch, Cottonwood, Magnolia, Dogwood
Schizophrenia
Schizophrenia is a complex journey, often marked by delusions, hallucinations, and distorted thoughts. An overactivity of dopamine in certain brain areas, particularly the mesolimbic pathway, is linked to schizophrenia. Too much dopamine can lead to some difficult symptoms like delusions and hallucinations. New research reveals that glutamate also has a big role to play - the main neurotransmitter that gets our neurons firing. Antipsychotic drugs are often used to treat schizophrenia by blocking the effects of dopamine or glutamate. Herbs like Ashwagandha, Ginkgo, Oatstraw, Siberian ginseng, and Holy basil are used to balance neurotransmitters and help relieve symptoms of schizophrenia. Calming nervines are a great way to ease stress and fear from those delusions or paranoia.
Herbal therapies ~ Ashwagandha, Ginkgo, St. John’s Wort, Oatstraw, Gotu kola, Holy Basil, Skullcap, Lemon balm, Blue vervain, Eleuthero (Siberian ginseng), Reishi, Lavender, Motherwort
Parkinsons Disease
Parkinson's disease is very serious progressive and degenerative neurological condition that mostly impairs motor function. It’s caused by the gradual death of neurons in the area of the brain called the substantia nigra, which is important for generating dopamine. Signs of Parkinson's disease include tremors, stiffness, bradykinesia (slow movement), and postural instability caused by a decrease in dopamine levels. The drug levodopa (L-DOPA) is a standard treatment for Parkinson's disease. It is a precursor to dopamine and can penetrate the blood-brain barrier. The brain then converts it into dopamine. Dopamine agonists and MAO-B inhibitors are two other methods that are used to treat Parkinsons. These drugs help raise dopamine levels and lower the amount that is broken down.
Herbal therapies ~ Ashwagandha, Ginkgo, Gotu kola, Holy Basil, Green tea, Turmeric, Rhodiola, Licorice, Skullcap, Oatstraw, Lemon balm, Blue vervain, Eleuthero (Siberian ginseng), Reishi, Rosemary, Ginger
Alzheimer’s Disease
Alzheimers is the most common form of dementia, where there is memory loss, confusion, and cognitive decline. The degeneration of neurons in the brain contributes to the cognitive issues seen in Alzheimers. Neurotransmitters acetylcholine and glutamate play a role in this disease. In Alzheimer’s we see lowered levels of acetylcholine, which is essential for memory and learning, and higher levels of glutamate. Damage or death to nerve cells occurs in ‘excitotoxicity’ when nerve cell receptors are overstimulated by abnormally high quantities of normally harmless neurotransmitters like glutamate and others. NMDA receptor antagonists like memantine can also help protect neurons from glutamate-induced excitotoxicity. Medications such as cholinesterase inhibitors (which prevent the breakdown of acetylcholine) are commonly used to treat symptoms of Alzheimer’s disease by increasing acetylcholine amounts in the brain.
Herbal therapies ~ Ginkgo, Ashwagandha, Schisandra, Blueberry, Lion’s mane mushroom, Reishi, Holy basil, Gotu kola, Rosemary, Sage, Lemon balm, Rhodiola, Ginseng, Turmeric, Green tea, Oatstraw, Peppermint, Lavender, Skullcap, St. John’s Wort, Ginger
ST JOHNS WORT
Increasing Serotonin
Plants of Joy & Calm
Serotonin (5-HT) is the well known neurotransmitter in our brains that keeps our mood more joyful and emotionally balanced. Serotonin is a mood booster, helping us feel calm, happy, and positive. Serotonin plays a huge role in our sleep, appetite, and digestion as well. When serotonin levels drop, it can lead to those heavy feelings of depression, anxiety, and irritability. Check out these amazing herbs that can boost your serotonin levels!
I’ve recommended St. John’s Wort (Hypericum perforatum) to people for many years as an antidepressant. It is also a general nervous system restorative, increasing nerve cell regeneration, and balancing to multiple neurotransmitters. St. John’s Wort inhibits the reuptake of serotonin, similar to how selective serotonin reuptake inhibitors (SSRIs) work, and should not be combined with any medications that also increase serotonin. St. John’s Wort also effects other neurotransmitters like dopamine and norepinephrine, all of which effect mood and can reduce depression. I recommend starting with 2 droppers full of tincture in water, going up to 3 as needed 2-3x a day. The liquid capsules (tincture in a capsule) are also effective, and I’ve loved the New Chapter and Gaia brands. St. John’s wort can interact with birth control pills and make some people more sensitive to the sun. Interestingly St. John’s Wort oil is helpful used topically for burns, as well as helping to heal damaged nerve tissue topically.
Rhodiola (Rhodiola rosea) root can also balance neurotransmitters, reduce stress, increase serotonin, and reduce feelings of depression. Rhodiola effects serotonin by modulating its receptors and reducing the breakdown of serotonin by enzymes. As an adaptogen it can increase energy levels, regulate the stress response, and lower fatigue for people with adrenal burn out. Some people find rhodiola a little too stimulating, so I recommend starting with a lower dose such as 1-2 droppers full in water. You can increase the dose until someone feels the effect without also feeling jittery or causing any headaches. The tea is also low dose - I recommend only 1 tsp. per quart of hot water steeped for 30 minutes or decocted for 10 minutes on low heat.
Ashwagandha (Withania somnifera) root also directly affects serotonin receptors similar to how selective serotonin reuptake inhibitors (SSRIs) work. It can increase serotonin levels in certain brain regions such as the hippocampus, which is connected to our moods as well as memory. I think Ashwagandha is amazing for depression, anxiety, and regulating stress. Ashwagandha can also can increase the availability of GABA (gamma-aminobutyric acid), which helps us feel calm and encourages relaxation. It is stabilizing to dopamine levels, helping to regulate moods, increase brain function, and lower stress. I recommend 1-3 droppers full of the tincture in water, lessening or increasing the dose based on the person and desired effects.
Schisandra (Schisandra chinensis) has always felt like the happy berry to me. It definitely improves the mood, lifts our spirits, energizes, and can clear away the blues. Schisandra has been shown in studies to enhance serotonin receptor sensitivity and increase serotonin levels in the brain. The sour berry has antidepressant effects, known to increase serotonin levels in the hippocampus and cortex, regions of the brain involved in mood regulation and brain function. Schisandra regulates our stress response as an adaptogen, and is especially helpful for adrenal burnout. I love schisandra for increasing energy levels, reducing anxiety, fatigue, and adrenal burn out. I recommend 3 droppers full of the tincture in water, lessening or increasing the dose based on the person and desired effects.
Ginkgo (Ginkgo biloba) can increase serotonin levels and help relieve depression or anxiety by regulating multiple neurotransmitters. This incredible tree can increase the concentration of serotonin in the brain especially the cerebral cortex, which is involved with brain function and mood. Ginkgo affects serotonin levels primarily through its action on serotonin receptors (5-HT1A and 5-HT2A receptors) and by increasing or modulating serotonin levels in the brain. Ginkgo also increases blood flow to the brain, which has been shown to support neurotransmitter activity (including serotonin). By improving circulation to the brain, the regions responsible for emotional regulation and mood such as the prefrontal cortex and hippocampus receive the oxygen and nutrients they need, which supports overall neurotransmitter balance. I recommend 1-3 droppers full of the tincture in water, lessening or increasing the dose based on body size and effects. Always start with the lower dose and increase.
GINKGO
Herbs Affecting Dopamine
Feeling that rush of happiness? It's often about those dopamine hits! We just can't help but chase that feel-good vibe again and again! Feels a little like a wild ride…
Dopamine is a neurotransmitter that effects our brain, mood, body, and behavior greatly. It is part of our brain’s reward pathway, which means it motivates us to certain behavior based on feeling pleasure and “reward” from something we do that feels good. Dopamine releases in a rush, and we then want to repeat the behavior that gave us the blast of feel good chemical… A bit like being on drugs! Dopamine can cause all kinds of repeated behaviors such as addiction to drugs, social media likes, eating delicious foods, addictive relationships, binge-watching your favorite show, achieving goals we set, or simply doing something we love to do. Dopamine also effects our ability to focus, think, plan, work on our goals, be excited and interested in anything. It helps us stay motivated and focused by creating a sense of reward when we accomplish something. Balanced dopamine can make us feel happy, motivated, and in control of our actions. A lack of dopamine can cause issues with focus, thinking clearly, depression, inability to feel pleasure, or to be in control of addictive behaviors.
Dopamine also effects the endocrine system in many ways including reducing insulin, increases urination, dilates our blood vessels, and reduces our immune response, (which is our white blood cell activity). It is a crucial neurotransmitter involved in our movement and coordination, which is why a lack of dopamine is linked to conditions like Parkinson's disease.
GINKGO
Ginkgo biloba is one of our most powerful brain and neural tonics, helping to rewire nervous system communication, support brain function, repair nerve damage, and balance neurotransmitters. Ginkgo improves dopamine function, enhances dopamine transmission, and protects dopamine neurons from oxidative stress. One of its key mechanisms is enhancing blood flow to the brain, which supports dopamine production and protects dopamine-producing neurons. Ginkgo is used to treat Alzheimer's disease and cognitive decline, where dopamine deficits play a role in the progression of these conditions. Ginkgo's antioxidant properties help protect the brain from free radical damage, which can mess up dopamine signaling. Ginkgo is neuroprotective in general as a strong antioxidant, preventing brain and neural degeneration. It’s used primarily to improve cognitive function and memory, especially in the elderly folks with conditions like dementia.
St. John’s Wort is best known for its use in treating mild to moderate depression, primarily due to its ability to modulate neurotransmitters like serotonin and dopamine. The herb increases dopamine availability in the brain by inhibiting its reuptake, which can help improve mood and emotional stability. St. John’s Wort has been studied extensively for its antidepressant properties and is often used as a natural alternative to pharmaceutical antidepressants for individuals with dopamine-related mood disorders .
Rhodiola rosea is an adaptogenic herb that helps the body cope with stress and fatigue by balancing neurotransmitters, including dopamine. It has been shown to improve mood, cognitive function, and energy levels by increasing dopamine production and enhancing the brain's ability to respond to stress. Rhodiola is particularly beneficial for individuals dealing with chronic stress and burnout, as it supports both physical and mental stamina . Animal studies have indicated that Rhodiola increases dopamine levels in the hippocampus and prefrontal cortex, improving mood and cognitive performance.
ASHWAGANDHA
Turmeric, widely known for its anti-inflammatory properties, also affects dopamine levels in the brain. Its active compound, curcumin, has been shown to increase dopamine by preventing its breakdown and reducing inflammation in the brain. Chronic inflammation is known to negatively impact dopamine production and receptor sensitivity, making curcumin a valuable tool for improving mood and cognitive function. Studies suggest that curcumin may be beneficial in treating conditions such as depression and Parkinson’s disease, where dopamine deficits are common.
Ashwagandha is another adaptogenic herb that has shown promise in enhancing dopamine levels. It helps reduce stress by modulating the hypothalamic-pituitary-adrenal (HPA) axis, which influences the body’s stress response. By reducing cortisol, the stress hormone, ashwagandha helps restore balance to neurotransmitter systems, including dopamine. Research indicates that ashwagandha increases dopamine receptor density in the brain, improving dopamine signaling and enhancing mood and cognitive function . This herb is often used to manage anxiety, depression, and stress-related disorders.
Panax ginseng, also known as Korean ginseng, is widely regarded for its ability to boost physical energy, improve cognitive function, and enhance mental clarity. It works by promoting the release of dopamine and protecting dopamine-producing neurons from damage. Ginseng has been used traditionally to treat fatigue and mental fog, and its effects on dopamine make it beneficial for individuals with mood disorders, such as depression and anxiety. Studies show that ginseng improves cognitive performance and may protect against neurodegenerative diseases by stabilizing dopamine levels.
GREEN TEA
Green tea is rich in L-theanine, an amino acid that increases dopamine release and causes relaxation without causing drowsiness. L-theanine can improve attention and focus by increasing dopamine levels in the brain. I’m personally obsessed with matcha and when I was dealing with a lot of whole body inflammation with Lyme, I drank a strong matcha latte I made at home daily. My favorite matcha that’s a much higher grade than most others and you can find it here. The polyphenols in green tea are strong antioxidants, lowering inflammation and oxidative stress in the body that can damage dopamine-producing neurons. Drinking green tea regularly helps us with good brain function, focus, and improved mood.
Holy Basil (Tulsi) is an adaptogen we know and love. It’s revered in India and used extensively in Ayurvedic medicine for its ability to support mental health and lower stress. Studies show tulsi balances neurotransmitters and regulates healthy amounts of dopamine. Tulsi can help us have more emotional balance, mental clarity, and healthy brain function. It’s especially restorative for people dealing with the effects of chronic stress, depression, or anxiety disorders. Holy basil can protect the brain from oxidative stress, prevent neural degeneration as we age, and increase dopamine levels. In general tulsi is anti-depressant, mood-enhancing, and neuroprotective… A major reason why we love it so much. I recommend a tincture or glycerite dose of 2-3 droppers full in water 2-3x a day for 2-3 months to see the most benefit.
MACA
Maca root is another adaptogenic herb known for its ability to boost energy, improve mood, and support hormonal balance. It has been shown to enhance dopamine levels, improving mood and motivation. Maca is often used to increase endurance, improve sexual function, and combat stress-related fatigue, making it a valuable tool for balancing dopamine and supporting mental health .
Licorice root contains compounds that may slow the breakdown of dopamine, allowing it to remain active in the brain for longer periods. By enhancing dopamine’s effects, licorice root can help improve mood, motivation, and energy levels. However, licorice root should be used cautiously, as excessive consumption can lead to elevated blood pressure due to its effects on cortisol metabolism.
Herbs Affecting Norepinephrine
Norepinephrine (Noradrenaline) is both a neurotransmitter and a hormone that is released during times of stress and initiates the body’s fight-or-flight response. Norepinephrine prepares the body for action by increasing heart rate, blood pressure, and alertness. Low levels of norepinephrine can lead to conditions such as depression and attention deficit hyperactivity disorder (ADHD), while high levels are linked to stress and anxiety.
Rhodiola can increase norepinephrine levels in the brain, which enhances focus, memory, and energy, especially in individuals dealing with the burnout effects of long term stress and mental exhaustion. This is why it can feel a bit overstimulating to some folks, so take this one in small amounts to start. Panax Ginseng also increases the release of norepinephrine, increasing alertness, focus, mental clarity and physical performance. This is why ginseng can also feel too stimulating for some, so also start with a low dose to begin with. Studies have shown that ginseng enhances norepinephrine transmission in the brain, which can help reduce fatigue and increase mental stamina, especially for people dealing with stress or declining brain function.
Ashwagandha also can help increase norepinephrine by enhancing the brain's sensitivity to this neurotransmitter, which can improve cognitive performance, mood, and attention. Thankfully it is also a nervine so it isn’t overstimulating. This makes Ashwagandha great for managing anxiety, stress, and ADHD-related symptoms. Green tea contains L-theanine, an amino acid that helps us relax. L-theanine balances norepinephrine by regulating its release in the brain, helping with focus and reducing stress-induced overstimulation. Ginkgo has also been shown in studies to increase norepinephrine release, improving focus and mental clarity, helpful for people with poor brain function and ADHD.
SCHISANDRA
Schisandra can also help improve focus, attention, and mental endurance by modulating norepinephrine and other neurotransmitter pathways. This beloved berry regulates the release of norepinephrine, lowering our stress response and supporting brain function. Siberian ginseng, or Eleuthero, is another adaptogenic that enhances mental and physical stamina. It works partly by increasing norepinephrine levels, which increases focus, energy, and brain function - especially for folks under stress or experiencing burn out.
Holy Basil can also increase norepinephrine levels, increasing focus, brain function, and supporting emotional regulation. Rosemary is another mint with neuroprotective effects that support mental clarity, focus, and memory by enhancing norepinephrine and dopamine activity in the brain. It is often used as a natural remedy for improving brain function. While it primarily affects GABA and serotonin, passionflower also modulates norepinephrine levels, helping to balance the body’s stress response. It supports relaxation without making us fall asleep, increasing focus and brain function, especially if anxiety is making it hard to focus.
St. John’s Wort also balances norepinephrine levels by inhibiting its reuptake in the brain. This is part of how it helps improve mood, focus, and attention in people with depression and anxiety. St. John’s wort balances multiple neurotransmitters that can help uplift our mood and lower stress. Gotu Kola improves brain function and reduces anxiety by increasing norepinephrine and serotonin levels bringing increased mental clarity, focus, and relaxation. I love the earthy grounding feel of gotu kola, and it’s used extensively in Asia as a nervous system and brain tonic. Gotu Kola’s neuroprotective properties improve memory and attention when used long term.
Maca also balances norepinephrine by enhancing neurotransmitter balance in the brain, improving focus and balancing our stress response. I find it stimulating and energizing, as well as grounding and regulating to our stress response. Yerba Mate is a stimulant herb commonly used to boost energy, focus, and mental clarity partly because it contains caffeine, which increases norepinephrine and dopamine levels in the brain. Caffeine in coffee and tea is a well-known stimulant that also increases norepinephrine and dopamine levels in the brain. Caffeine boosts our attention and mental energy, improving cognitive performance and mental focus.
SAGE
Herbs that Affect Acetylcholine
Acetylcholine (ACh) is another well known neurotransmitter affecting brain function, muscle contraction, memory, learning, and cognition. In the brain and spinal cord it facilitates cognitive processes, and in the body it activates our muscles. Acetylcholine deficiency is linked to cognitive decline in Alzheimer's disease and other neurodegenerative disorders. Certain herbs can help increase acetylcholine levels, enhance its release, or inhibit its breakdown. These herbs are natural support for improving brain function, reducing cognitive degeneration, and improving our memory.
Ginkgo biloba is widely known for its cognitive enhancing and neuroprotective properties. It increases blood flow to the brain and increases acetylcholine activity by protecting neurons and enhancing acetylcholine receptor function. Ginkgo has been shown to improve memory, attention, and cognitive performance, especially in individuals with cognitive impairments or age-related decline . Its ability to enhance acetylcholine signaling makes it helpful in preventing or slowing the progression of neurodegenerative diseases.
Sage has been traditionally used to enhance memory and mental clarity, and scientific studies confirm its ability to inhibit acetylcholinesterase, which helps increase acetylcholine levels in the brain. Sage has been shown to improve cognitive performance, especially in people with Alzheimer's disease and age-related memory decline, making it a great plant for neuroprotection and memory.
Rosemary is a wonderful plant as well as sage to increase memory. Studies show it increases acetylcholine levels. Carnosic acid, one of its active compounds, protects acetylcholine receptors from oxidative stress and inhibits acetylcholinesterase (ACHE), the enzyme that breaks down acetylcholine. Rosemary has been traditionally used to boost memory and focus, and scientific research supports its neuroprotective and cognitive-enhancing properties.
Lemon Balm is a calming herb used for hundreds of years for anxiety and brain function. It has been shown to inhibit acetylcholinesterase, increasing acetylcholine levels and improving memory and attention. Lemon Balm’s ability to uplift our mood and brain function makes it great for managing stress-related cognitive decline and increasing focus.
Peppermint is known for its stimulating effects on the brain, which I’ve loved for years. Research shows it can also enhance acetylcholine activity and improve attention, memory, brain function, and sustained focus on tasks. It works by supporting neurotransmitter function including acetylcholine, increasing mental clarity, memory, and attention. I breath in peppermint essential oil when I need to stay awake and focus on driving or work. It’s incredibly helpful!
Gotu Kola is a traditional Ayurvedic herb we’ve mentioned many times already, used for enhancing memory, cognition, and overall brain health. It works by increasing acetylcholine levels and supporting synaptic communication. Gotu Kola has been shown to improve memory and learning in both animal and human studies, making it an important plant for brain function especially with age-related decline. I love mixing it with ginkgo and adaptogens like siberian ginseng or ashwangandha for memory.
Ashwagandha is an adaptogen that improves brain function by modulating various neurotransmitters, including acetylcholine. Research shows Ashwagandha increases acetylcholine receptor activity and promotes acetylcholine release, supporting memory, clear thinking, and good brain function. It is also used to manage stress as one of our best adaptogens for the nervous system, lowering anxiety (as a nervine), and addressing neurodegenerative disorders, especially where acetylcholine depletion is a factor.
Lion's Mane is a medicinal mushroom well known for its neuroprotective and cognitive-enhancing effects. It promotes the growth of nerve cells and supports the production of acetylcholine by enhancing the production of nerve growth factor (NGF), which is essential for the health of cholinergic neurons. Brain cells called cholinergic neurons send information with the help of the neurotransmitter acetylcholine. One of the first signs of Alzheimer's disease is the loss or failure of cholinergic neurons in the basal forebrain. Lion’s Mane has been shown to improve memory, learning, and cognitive function, especially because it helps in maintaining acetylcholine levels.
Turmeric contains the compound curcumin, and gives us neuroprotective effects by increasing acetylcholine levels and reducing neuroinflammation. Curcumin has been found to inhibit acetylcholinesterase, which increases acetylcholine availability in the brain. Turmeric can help improve memory and brain function, especially in neurodegenerative conditions like Alzheimer's.
Green tea contains L-theanine and catechins, both of which offer neuroprotective benefits and support acetylcholine function. Green tea has been shown to increase brain function, improve memory, and protect neurons from oxidative stress, which can impair acetylcholine signaling. Regular consumption of green tea has been linked to better cognitive function and a reduced risk of cognitive decline. I would just make sure that you buy organic green tea since herbicides are neurotoxins folks!
Blueberries and blueberry leaf are rich in antioxidants, especially flavonoids, which enhance brain function and acetylcholine. Studies have shown that blueberries improve memory and cognitive performance by supporting acetylcholine signaling and protecting cholinergic neurons from oxidative damage. They are also very anti-inflammatory, which I’ve felt in my own body for years. I eat tons of blueberries, add them to smoothies, and make tinctures from the leaves. I can feel the reduction in body and brain inflammation from them the day I consume them.
Panax ginseng is another adaptogen that supports cognitive function by enhancing acetylcholine levels and improving synaptic transmission. Ginseng has been shown to improve memory, focus, and mental clarity, making it great for age-related memory decline. You can use it for Alzheimers and dementia, or general brain function for anyone. Ginseng has been used in Asia for thousands of years for its anti-aging effects including benefiting cognitive function especially for elders.
LEMON BALM
Relaxing with GABA
The chill out neurotransmitter
GABA, aka Gamma-Aminobutyric Acid, is the chillout neurotransmitter in our brain that helps our nervous system relax. GABA is a lot of what we need to feel calm and focused! In our brain and spinal cord, GABA plays a crucial role in keeping neurons in check and preventing them from firing too fast. This helps to calm the nervous system down overall. Anxiety disorders, epilepsy, and insomnia can all be connected to low levels of GABA. When we are feeling nervous, stressed, or overwhelmed we need the calming effect of GABA to keep our mind in check. GABA makes it less likely for nerve cells to send messages when it binds to receptors on our neurons. When your brain is low on GABA, it can get a little too hyper! This can lead to feelings of worry, restlessness, or even some serious issues like seizures. GABA is essential for that inner calm we all crave. It will help with anxiety disorders, fears, and those endless cycles of worried thoughts. GABA brings peace for a good night's sleep and a balanced mind.
There are many herbs that can help raise GABA levels, which calms and soothes the nervous system and helps us relax. Passionflower, valerian root and skullcap are ultimate calming herbs that raise GABA. Perfect for managing anxiety, relaxing your body, and lowering stress levels. These amazing herbs boost the activity of inhibitory neurotransmitters like GABA, creating a perfect balance against glutamate, the one that gets our brains buzzing! Valerian helps boost GABA levels by slowing down its breakdown. We use it to calm those restless nights and easing anxiety. Passionflower is well known to help us chill out, calm anxiety, and boost sweet dreams by ramping up GABA in the brain. keeping the central nervous system all zen. Lemon balm is a beloved herb for GABA support helping us to chill out and lower anxiety. It’s super mild yet very effective, calming without the drowsiness. Ashwagandha also increases GABA, helping our bodies relax and adapt to stress.
Herbs that affect Glutamate
In your brain, glutamate is the most abundant excitatory neurotransmitter. An excitatory neurotransmitter excites or stimulates a nerve cell, making it more likely that the chemical message will continue to move from nerve cell to nerve cell and not be stopped. Glutamate is essential for proper brain function but high levels can cause lowered GABA levels, anxiety, stress, pain, and difficulty relaxing. Glutamate stimulates the brain, while GABA calms it down, and both can be out of balance. When glutamate is too high and GABA levels are too low, we can experience chronic pain (as in fibromyalgia), chronic fatigue, sensitivity to pain, anxiety, restlessness, brain fog, insomnia, mental exhaustion, overstimulation, and low energy. Glutamate is also needed for making GABA.
To modulate glutamate activity, certain herbs can protect against glutamate excitotoxicity and increase overall brain health. Herbs such as ginkgo biloba contain antioxidants and neuroprotective compounds that can modulate NMDA receptors, reducing excessive glutamate release and providing a buffer against oxidative stress. Ginkgo biloba’s can help protect neurons from glutamate-induced toxicity. Ginseng (Panax ginseng) is another herb known for its neuroprotective properties. It contains ginsenosides that regulate neurotransmitter release, including glutamate, and help prevent excitotoxic damage. Ginsenosides have an inhibitory effect on glutamate toxicity, which can help folks with neurodegenerative conditions.
Turmeric, Rosemary, Sage, and Green tea have been also shown to regulate glutamate and their antioxidant effects counteract glutamate excitotoxicity. Both have antioxidant and anti-inflammatory properties that support brain health and protect neurons from damage. Ashwagandha also reduce stress-induced glutamate spikes and increase relaxation. Valerian and skullcap have also been shown to reduce glutamate activity in overactive neurons, contributing to a balanced neurochemical environment conducive to cognitive health.
Anxiety Disorders
Anxiety caused by neurotransmitter imbalances are common and often caused by dysfunction in the neurotransmitter systems responsible for regulating fear, worry, and our stress response. The neurotransmitter GABA helps reduce anxiety by lowering neural excitability and promoting calmness. Low levels of GABA are associated with increased anxiety and fear responses. Low levels of serotonin and dopamine also play an important role in causing anxiety. Norepinephrine is involved in the body's "fight or flight" response and overactivity in the norepinephrine system can cause increased feelings of stress and anxiety. Anxiety disorders are typically managed with medications such as SSRIs (which increase serotonin) or benzodiazepines (which enhance GABA). Behavioral therapies, mindfulness practices, and exercise can also help improve neurotransmitter balance and lower anxiety.
We also have an incredible numbers of awesome nervine herbs that can balance these neurotransmitters and calm us down. They should be used regularly 2-3 times a day for months at a time.
Nervines ~ Passionflower, Skullcap, Blue vervain, Motherwort, Tilo, Linden, Peach, Kava kava, Oatstraw, Valerian, St. john’s wort, California poppy, Wild lettuce, Mugwort, White Peony, Lavender, Sage, Egyptain blue lotus, Cannabis (with correct dose), Elder flower, Rose, Wild cherry, Lemon balm, Chamomile, Ginger, and the many others…
OATSTRAW
Herbal Therapy
for ADHD
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental condition that has been closely linked to imbalances in neurotransmitters such as dopamine and norepinephrine, which effect our concentration, motivation, and executive functioning. In the brains of people with ADHD, there is often insufficient dopamine in regions like the prefrontal cortex, which is the area of our brain responsible for regulating behavior, decision-making, and focus. Dopamine helps signal rewards and motivation. When its levels are too low, people struggle with shifting attention, maintaining attention, resisting distractions, or following through on tasks. Dopamine deficiency can explain why people with ADHD often find it difficult to stay focused on activities that do not provide immediate rewards or stimulation. It can cause difficulty with attention, hyperactivity, impulsivity, mood regulation, and organization. For example, a child or teen with ADHD may have trouble in school and home with paying attention, concentrating, losing things, following directions, sitting still, acting without thinking, or getting mad and frustrated easily.
Many people with ADHD (like myself) experience a form of hyperfocus than can feel like a superpower but also comes with a lot of down sides. Hyperfocus refers to an intense fixation on an interest or activity for an extended period of time. People who experience hyperfocus often become so engrossed they block out the world around them. Children and adults with ADHD often exhibit hyperfocus when working intently on things that interest them. A better way to look at it is that people with ADHD have a disregulated attention system.
Like distractibility, hyperfocus is thought to result from abnormally low levels of dopamine, a neurotransmitter in the brain’s frontal lobes. This dopamine deficiency makes it hard to “shift gears” to take up boring-but-necessary tasks. Children and adults with ADHD have difficulty shifting attention from one thing to another. If they’re doing something they enjoy or find psychologically rewarding, they’ll tend to persist in this behavior after others would normally move on to other things. The brains of people with ADHD are drawn to activities that give instant feedback. The intense concentration is actually a coping mechanism.
Hyperfocus a way of dealing with distraction. People with ADHD can intentionally go into a state of intense focus to get work done. Kids do the same thing unconsciously when they’re doing something pleasurable, like watching a movie or playing a computer game. Often they aren’t even aware that they’re focusing so intensely. There’s nothing inherently harmful about hyperfocus. In fact, it can be an asset. Some people with ADHD, for example, are able to channel their focus on something productive, such as a school- or work-related activity. Others allow themselves to hyperfocus on something as a reward for completing a dull but important task. Many scientists, writers, and artists with ADHD have had very successful careers, in large part because of their ability to focus on what they’re doing for hours on end.
Norepinephrine also plays a significant role in ADHD, as it helps with alertness and arousal. Inadequate norepinephrine signaling can result in difficulties with sustaining attention, controlling impulses, and regulating emotional responses. Both neurotransmitters interact closely in the prefrontal cortex, and their dysfunction contributes to the hallmark symptoms of ADHD - inattention, hyperactivity, and impulsivity. Treatments for ADHD, such as stimulant medications like methylphenidate (Ritalin) and amphetamine salts (Adderall), work by increasing the availability of dopamine and norepinephrine in the brain, helping to improve focus and control hyperactive behavior. These medications either block the reuptake of these neurotransmitters or promote their release, restoring balance and reducing ADHD symptoms. Non-stimulant medications, such as atomoxetine, target norepinephrine specifically, offering another therapeutic option.
Some studies suggest that serotonin might influence mood and emotional regulation in people with ADHD, contributing to the emotional dysregulation often seen in some people. Overall, neurotransmitter imbalances are central to the pathophysiology of ADHD, and understanding these dysfunctions has paved the way for effective pharmacological treatments that restore neurotransmitter balance, helping individuals with ADHD manage their symptoms more effectively.
his dopamine deficiency contributes to the reduced ability to experience reward from everyday activities, making it difficult for those with ADHD to sustain attention or stay motivated unless the task is highly stimulating or immediately rewarding. The prefrontal cortex, which is crucial for planning, decision-making, and impulse control, relies heavily on balanced dopamine signaling to function properly. In ADHD, this system is underactive, leading to poor impulse regulation, distractibility, and difficulty maintaining focus. As a result, individuals with ADHD are more likely to seek out high-reward activities, such as novelty or risk-taking behaviors, to compensate for the lower dopamine activity in the reward pathway.
Scientists have shown that there are differences in the brains of children with ADHD and that some of these differences change as a child ages and matures. Research has shown that some structures in the brain in children with ADHD can be smaller than those areas of the brain in children without ADHD.
The brain is an organ that controls thinking, feeling, and behavior. The brain is divided into sections called lobes. The front of the brain behind the forehead is the frontal lobe. The frontal lobe is the part of the brain that helps people to organize, plan, pay attention, and make decisions. Parts of the frontal lobe may mature a few years later in people with ADHD. The frontal lobe is the area of the brain responsible for Problem Solving Memory Language Motivation Judgment Impulse control Social behavior Planning Decision-making Attention Ability to delay gratification Time perception organization Planning and organization Focus and attention Self-monitoring and self-control Memory Communication Problem-solving Impulse control Language Social behavior Motivation Judgment
The brain is made up of nerve cells called neurons that transmit signals in the brain. Signals travel through the brain in groups of nerve cells called "networks." Researchers have identified several major networks that work differently in people with ADHD. These networks are involved in reward, focus, planning, attention, shifting between tasks, and movement.
One of the most significant differences between an ADHD brain vs. a normal brain is the level of norepinephrine (a neurotransmitter). Norepinephrine is synthesized from dopamine. Since the two go hand-in-hand, experts believe that lower levels of dopamine and norepinephrine are both linked to ADHD. An imbalance in the transmission of dopamine in the brain may be associated with symptoms of ADHD, including inattention and impulsivity. This disruption may also interfere with the dopamine reward pathway, changing how the ADHD brain perceives reward and pleasure.
The structure of the ADHD brain can also differ from a non-ADHD brain in certain areas, including the following:
Frontal cortex: This region regulates your behavior, emotions, and attention.
Limbic regions: The limbic system influences your emotions and motivation. ADHD-related changes to this area of the brain can contribute to hyperactivity, inattention, and poorer decision-making.
Basal ganglia: The basal ganglia is responsible for motor learning (picking up a particular skill through practice or experience). It also helps regulate your behavior, emotions, and ability to plan, focus, and multi-task—all of which are affected by ADHD.
Another significant difference involves the default mode network (DMN) of the brain. The DMN activates when you’re daydreaming or not focused (or unable to focus) on a task or activity. In ADHD, the DMN is more often activated. As a result, you may feel that your focus is constantly being pulled away from the task at hand toward unrelated thoughts.
An ADHD brain differs from a neurotypical one in many ways—from the size and activity levels of certain regions to the chemical signals traveling throughout the brain. Because of these differences, you may find it challenging to organize, plan, focus, and manage your emotions with ADHD. Let’s dive deeper into what the structure, network, and chemistry of an ADHD brain look like.
In an ADHD brain, imbalances in the function and structure of these networks may cause the brain to transmit messages less effectively.
Research has found deficits in the neural networks linked to attention and executive function in children and adults with ADHD. This may affect your ability to organize, prioritize, plan, focus, remember instructions, and work toward your goals.
In addition, ADHD may alter the network connections between your prefrontal cortex (a section of the frontal lobe) and other areas of the brain. Scientists believe this is associated with poor planning, distractability, impulsivity, and forgetfulness in ADHD.
Other deficits in networks of the frontal and parietal lobes of the brain can affect your attention, motivation, and ability to control your responses and predict the difficulty of a task. It may also change how you make decisions based on the perceived rewards.
This could make it more difficult to retain the information needed to complete tasks successfully. It may also impair your inhibitory control, which is how well you can suppress distractions, urges, or behaviors that interfere with your goals.
Meanwhile, dopamine helps us regulate our emotions and is linked to feelings of pleasure and reward. In ADHD, there might be lower levels of dopamine in the brain. This makes it harder to maintain motivation, especially when the rewards seem small or not immediate. ADHD brains tend to favor short-term, smaller rewards over long-term, more significant ones.
dysfunction in the “brain reward cascade,” especially in the dopamine system, causing a low or hypo-dopaminergic trait, the brain may require dopamine for individuals to avoid unpleasant feelings. This high-risk genetic trait leads to multiple drug-seeking behaviors, because the drugs activate release of dopamine, which can diminish abnormal cravings. Moreover, this genetic trait is due in part to a form of a gene (DRD2 A1 allele) that prevents the expression of the normal laying down of dopamine receptors in brain reward sites. This gene, and others involved in neurophysiological processing of specific neurotransmitters, have been associated with deficient functions and predispose individuals to have a high risk for addictive, impulsive, and compulsive behavioral propensities. It has been proposed that genetic variants of dopaminergic genes and other “reward genes” are important common determinants of reward deficiency syndrome (RDS), which we hypothesize includes ADHD as a behavioral subtype. We further hypothesize that early diagnosis through genetic polymorphic identification in combination with DNA-based customized nutraceutical administration to young children may attenuate behavioral symptoms associated with ADHD. Moreover, it is concluded that dopamine and serotonin releasers might be useful therapeutic adjuncts for the treatment of other RDS behavioral subtypes, including addictions.
Ginkgo biloba is thought to improve symptoms of ADHD by enhancing blood flow to the brain and providing antioxidant protection to neurons. Ginkgo works by increasing cerebral circulation and promoting the release of neurotransmitters such as dopamine and acetylcholine, both of which are critical for attention and focus. Studies have shown that ginkgo may help improve attention, memory, and executive functioning, which are often impaired in individuals with ADHD. In a double-blind, placebo-controlled study on children with ADHD, Ginkgo biloba was found to improve attention and reduce hyperactivity, though the effects were modest compared to stimulant medications. * Use with caution combined with blood thinners.
Panax ginseng has been used for centuries to boost mental clarity, focus, and energy. In the context of ADHD, Panax ginseng may improve symptoms by increasing dopamine production and enhancing cognitive function. Research suggests that Panax ginseng may help improve attention span, impulse control, and hyperactivity in children and adults with ADHD. A double-blind, placebo-controlled study found that children who were treated with a combination of ginseng and ginkgo experienced significant improvements in cognitive function and behavioral symptoms compared to the placebo group. The effects of ginseng on ADHD are believed to stem from its ability to increase dopamine levels in the brain, which are often deficient in individuals with ADHD. Moreover, ginseng has neuroprotective and anti-fatigue properties, which may help individuals with ADHD manage the cognitive and emotional exhaustion that often accompanies the disorder.
Rhodiola rosea is another adaptogenic herb that has gained popularity for its ability to enhance cognitive function, mental endurance, and stress resilience. Rhodiola is known for its anti-fatigue and anti-stress effects, which are particularly beneficial for individuals with ADHD who may struggle with cognitive fatigue and emotional dysregulation. By balancing neurotransmitters like dopamine and serotonin, Rhodiola helps improve focus, motivation, and emotional regulation. Several studies have demonstrated the benefits of Rhodiola in improving cognitive performance and reducing mental fatigue in individuals with ADHD. In one clinical trial, participants who took Rhodiola supplements reported enhanced mental clarity, better concentration, and reduced symptoms of burnout. Rhodiola's effects on dopamine pathways make it particularly useful for individuals with ADHD. Rhodiola’s ability to modulate the hypothalamic-pituitary-adrenal (HPA) axis helps reduce stress-induced cognitive decline, which can exacerbate ADHD symptoms.
Gotu kola is a traditional medicinal herb that has been used for centuries in Ayurvedic and Traditional Chinese Medicine to enhance cognitive function, memory, and circulation. In the context of ADHD, Gotu kola’s ability to improve brain function and promote calmness makes it a valuable herb for managing symptoms such as hyperactivity and inattention. Gotu kola works by increasing blood flow to the brain, enhancing neuronal communication, and supporting the production of neurotransmitters like serotonin and dopamine, both of which are critical for attention and mood regulation. Research on Gotu kola has shown promising results in improving memory retention, focus, and mental clarity in individuals with cognitive impairments, including those with ADHD. Gotu kola is also known for its calming effects, making it particularly beneficial for individuals with ADHD who struggle with impulsivity and hyperactivity. Its ability to promote relaxation without causing sedation makes Gotu kola an ideal herb for supporting focus and mental alertness in both children and adults with ADHD.
Ashwagandha, another prominent herb in Ayurvedic medicine, is classified as an adaptogen and is known for its ability to reduce stress, anxiety, and mental fatigue. In individuals with ADHD, chronic stress and anxiety can exacerbate symptoms such as inattention, impulsivity, and hyperactivity. By modulating the body's stress response and enhancing dopamine and GABA signaling, ashwagandha may help improve both cognitive function and emotional regulation in individuals with ADHD. Several studies have highlighted ashwagandha’s potential to improve attention and cognitive performance in individuals under stress, including those with ADHD. One randomized controlled trial found that children who took ashwagandha supplements experienced significant improvements in executive function, working memory, and attention span compared to the placebo group. Ashwagandha’s ability to balance the HPA axis and support neurotransmitter regulation makes it a promising natural remedy for managing the cognitive and emotional challenges associated with ADHD.
Passionflower is a calming herb traditionally used to treat anxiety, insomnia, and nervous tension. For individuals with ADHD, who often struggle with restlessness, impulsivity, and sleep disturbances, passionflower offers a gentle and natural way to promote relaxation and improve sleep quality. Passionflower works by enhancing GABAergic transmission, which helps calm neuronal activity and reduce hyperexcitability in the brain. Studies have shown that passionflower can be an effective natural remedy for reducing symptoms of hyperactivity and impulsivity in individuals with ADHD, particularly when combined with other herbs like valerian root. By promoting relaxation and supporting GABA function, passionflower helps reduce anxiety and restlessness, allowing individuals with ADHD to focus more effectively and feel more calm and grounded throughout the day. Additionally, passionflower's ability to improve sleep quality is particularly beneficial for individuals with ADHD who experience sleep disturbances, as poor sleep can exacerbate ADHD symptoms.
Valerian root is another herb commonly used to promote relaxation and improve sleep quality. In individuals with ADHD, particularly those who experience insomnia or restlessness at night, valerian root can be an effective herbal remedy for promoting calmness and restful sleep. Like passionflower, valerian works by increasing GABA activity in the brain, which helps to reduce hyperactivity and anxiety—common issues in individuals with ADHD, especially during the evening when winding down for sleep can be difficult. GABA is the brain’s primary inhibitory neurotransmitter, and its activation helps calm the nervous system, reducing overstimulation and promoting relaxation. Several studies have demonstrated valerian root’s efficacy in treating insomnia and restlessness, and it has been used historically as a sleep aid for individuals dealing with anxiety or stress. In the context of ADHD, valerian root may be particularly useful for individuals who struggle with sleep disturbances, which are often associated with poor attention and irritability during the day. Improving sleep quality through natural means such as valerian root may help alleviate some of the daytime cognitive challenges that individuals with ADHD face. Moreover, combining valerian with other calming herbs, such as lemon balm or passionflower, may enhance its effects on sleep and relaxation.
Skullcap is another herb traditionally used to treat nervous tension, anxiety, and insomnia, making it a valuable herb for individuals with ADHD who experience symptoms of emotional dysregulation and restlessness. Skullcap works by modulating GABA activity in the brain, similar to valerian and passionflower, which helps calm the nervous system and reduce overactivity. By enhancing GABAergic transmission, skullcap may reduce hyperactivity and impulsivity, allowing individuals with ADHD to feel more centered and focused. In addition to its calming effects, skullcap has neuroprotective properties, which may help protect the brain from oxidative stress and inflammation, both of which can contribute to cognitive deficits in individuals with ADHD. By reducing anxiety and promoting relaxation, skullcap helps support mental clarity and focus, making it a useful herb for managing the emotional and cognitive challenges associated with ADHD. While skullcap is generally considered safe, it should be used with caution in individuals taking medications that affect the central nervous system.
Lemon balm is a gentle herb known for its calming effects on the nervous system and its ability to improve cognitive function. For individuals with ADHD, lemon balm can help reduce symptoms of anxiety and restlessness, making it easier to focus and concentrate. Lemon balm works by modulating GABA activity and promoting the release of serotonin, which helps regulate mood and improve emotional stability. Research has shown that lemon balm can improve attention and memory in both children and adults, making it a valuable herb for supporting cognitive function in individuals with ADHD. Additionally, lemon balm’s anxiolytic properties make it particularly useful for individuals who experience social anxiety or nervous tension, both of which are common in individuals with ADHD. When combined with other herbs like valerian root or passionflower, lemon balm can enhance calmness and promote a more balanced state of mind.
St. John’s Wort is primarily known for its ability to treat mild to moderate depression, but it may also have benefits for individuals with ADHD who experience mood swings, emotional instability, or impulsivity. St. John’s Wort works by inhibiting the reuptake of serotonin, dopamine, and norepinephrine, thereby increasing the availability of these neurotransmitters in the brain. This mechanism is similar to that of antidepressant medications, though St. John’s Wort is considered a more natural alternative with fewer side effects. For individuals with ADHD, particularly those with comorbid depression or anxiety, St. John’s Wort may help improve mood regulation and reduce emotional volatility. However, it is important to note that St. John’s Wort can interact with a variety of medications, including antidepressants, birth control pills, and blood thinners, so it should be used with caution and under the guidance of a healthcare provider. Additionally, St. John’s Wort can increase sensitivity to sunlight, so individuals taking this herb should avoid excessive sun exposure.
Grape seed extract is a powerful antioxidant derived from the seeds of grapes, and it has been shown to have a variety of benefits for cognitive function and attention. Grape seed extract contains high levels of proanthocyanidins, which are potent antioxidants that protect the brain from oxidative stress and support healthy blood flow. By improving blood circulation to the brain, grape seed extract may enhance mental clarity, focus, and cognitive endurance in individuals with ADHD. In one study, grape seed extract was found to improve attention and impulse control in children with ADHD, suggesting that its antioxidant and neuroprotective effects may help support brain function. Additionally, grape seed extract has anti-inflammatory properties, which may help reduce neuroinflammation, a factor that is increasingly recognized as playing a role in ADHD. As a natural antioxidant, grape seed extract may be particularly beneficial for individuals with ADHD who experience cognitive fatigue or brain fog.
Oat straw, also known as wild green oat, is a nutrient-rich herb that has been traditionally used to support nervous system health and improve mental performance. Oat straw contains compounds such as avenanthramides, which have anti-inflammatory and antioxidant properties, helping to protect the brain from oxidative damage. In individuals with ADHD, oat straw may help improve focus, attention, and cognitive endurance by supporting dopamine production and promoting healthy brain function. Research has shown that oat straw can improve attention and working memory in both children and adults, making it a valuable herb for individuals with ADHD who struggle with inattention and impulsivity. Oat straw is also known for its calming effects, making it particularly beneficial for individuals who experience stress or anxiety. Its ability to nourish the nervous system and support cognitive function makes oat straw a useful natural remedy for managing ADHD symptoms.
Holy basil, also known as Tulsi, is an adaptogenic herb that has been used in Ayurvedic medicine for centuries to promote mental clarity, reduce stress, and support overall cognitive function. Holy basil is known for its ability to modulate the HPA axis, reducing the negative effects of chronic stress on the brain and body. In individuals with ADHD, chronic stress can exacerbate symptoms of inattention, impulsivity, and emotional dysregulation. Holy basil has been shown to improve focus, memory, and mental clarity by balancing neurotransmitters like dopamine and serotonin. Its ability to reduce cortisol levels makes it particularly beneficial for individuals with ADHD who experience anxiety or stress-related cognitive decline. Holy basil's anti-inflammatory and neuroprotective properties further support brain health, making it a valuable herb for managing ADHD symptoms and promoting overall mental well-being.
LINDEN
The Second Brain
The Enteric Nervous System in our Gut
The enteric nervous system (ENS) is a complex network of about 100 million neurons within the walls of the gastrointestinal tract (about the same amount as we find in the spinal cord). It controls digestive functions such as peristalsis (the movement of food through the intestines), secretion of digestive enzymes, and blood flow to the gut. The enteric nervous system communicates with the brain through the gut-brain axis, regulates the immune system and the health of our gut microbiom. The ENS primarily functions through neurotransmitters like acetylcholine, serotonin, and dopamine, which help regulate digestive processes and influence mood and emotions.
Up to 90% of the body’s serotonin is produced in the gut, highlighting the ENS’s role in both digestive health and mental well-being. Dysregulation of the ENS can lead to conditions such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and other functional GI disorders, where the interaction between the gut and the brain becomes impaired.
The ENS produces and utilizes many of the same neurotransmitters found in the brain, such as serotonin, dopamine, and acetylcholine. Serotonin, a neurotransmitter primarily known for its role in mood regulation, is found in significant quantities in the gastrointestinal (GI) tract. The gut microbiota, composed of trillions of bacteria residing in the gastrointestinal tract, plays a critical role in serotonin production and its influence on the nervous system. In fact, about 90-95% of the body’s serotonin is produced in the intestines, where it helps regulate various digestive processes such as bowel movements and the perception of pain or discomfort in the gut.
However, the serotonin produced in the gut does not directly reach the brain because it is blocked by the blood-brain barrier (BBB), a protective mechanism that shields the brain from many substances circulating in the bloodstream. Despite this, serotonin in the intestines can activate receptors on the vagus nerve, sending signals to the brain and influencing mood, stress responses, and even cognition. While serotonin itself does not cross the blood-brain barrier, its precursor, tryptophan, does. Tryptophan is an essential amino acid obtained through diet, and gut microbes can influence its metabolism. Once in the brain, tryptophan can be converted into serotonin, impacting mood and behavior.
The vagus nerve acts as a communication superhighway between the gut and the brain.
Gut bacteria plays a key role in the production and regulation of serotonin in the intestines.
The gut is home to a large portion of the body’s immune cells. The ENS plays a critical role in regulating the immune responses in the gut and maintaining the integrity of the intestinal lining, which acts as a barrier against pathogens. Serotonin from the gut can modulate the immune system, influencing the release of cytokines (immune signaling molecules). These cytokines can indirectly affect the brain, contributing to changes in mood, cognition, and mental health.
Research suggests that gut-derived serotonin can influence conditions such as anxiety, depression, and irritable bowel syndrome (IBS). Dysregulation of serotonin in the gut, often linked to gut microbiota imbalances, can contribute to both gastrointestinal and mental health disorders. For example, people with IBS often experience mood disorders, and this may be partly due to disrupted serotonin signaling along the gut-brain axis. In summary, while serotonin produced in the intestines does not directly enter the brain, it profoundly influences brain function through a network of neural, immune, and hormonal pathways that make up the gut-brain axis.
Serotonin (5-hydroxytryptamine, or 5-HT) is a neurotransmitter primarily recognized for its role in mood regulation, but it also has a wide range of functions in both the central nervous system (CNS) and the peripheral nervous system (PNS). Approximately 90-95% of serotonin is produced in the gastrointestinal (GI) tract, particularly by enterochromaffin cells, while the remaining serotonin is synthesized in the brain. Serotonin is synthesized from the essential amino acid tryptophan, which must be obtained through the diet. Tryptophan is converted to 5-hydroxytryptophan (5-HTP) by the enzyme tryptophan hydroxylase, and then to serotonin. In the brain, serotonin must cross the blood-brain barrier, meaning that its production and regulation are influenced by a delicate balance of dietary intake, enzymatic activity, and neurotransmitter regulation.
Research has shown that certain gut bacteria can stimulate the production of serotonin in the intestines, which then influences both gut health and central nervous system function.
Several specific bacterial species in the gut are involved in serotonin production. These bacteria either produce metabolites that serve as precursors for serotonin synthesis or directly influence the activity of enterochromaffin cells, which are responsible for releasing serotonin into the gut. Bifidobacterium and Lactobacillus: These bacteria produce metabolites that promote serotonin synthesis from tryptophan. Escherichia coli: This bacterium has been shown to affect serotonin biosynthesis by modulating tryptophan metabolism. Clostridium spp.: These bacteria influence serotonin production through their metabolic byproducts, including short-chain fatty acids (SCFAs).
Gut bacteria influence serotonin levels through the production of short-chain fatty acids (SCFAs), such as butyrate, acetate, and propionate. SCFAs act on the gut epithelium and the enteric nervous system (ENS) to promote serotonin release. These microbial metabolites can affect the permeability of the gut lining, immune system activity, and signaling to the brain through the vagus nerve.
In the CNS, serotonin plays a key role in mood regulation, learning, memory, and sleep. Low levels of serotonin are commonly associated with depression, anxiety, and mood disorders. Selective serotonin reuptake inhibitors (SSRIs), a class of antidepressants, work by increasing serotonin availability in the synaptic cleft, thus enhancing mood and emotional regulation. Mood Regulation: Serotonin modulates the activity of the limbic system, which includes structures like the amygdala and hippocampus that are involved in emotional processing. Serotonin is a precursor to melatonin, a hormone that regulates the sleep-wake cycle. Cognitive Function: Serotonin influences learning and memory by affecting the strength of synaptic connections.
The enteric nervous system (ENS), often referred to as the “second brain,” is a network of neurons embedded in the gut wall that controls gastrointestinal functions independently of the CNS. Serotonin promotes the contraction of smooth muscles in the intestines, facilitating digestion and the movement of food through the GI tract. Serotonin modulates pain perception in the gut, influencing conditions like irritable bowel syndrome (IBS), where serotonin levels are often dysregulated.
The vagus nerve is a key component of the gut-brain axis and plays a central role in transmitting signals between the gut and the brain. Serotonin produced in the gut can influence brain function via the vagus nerve. Serotonin released in the gut stimulates vagal afferent neurons, which relay signals to the brainstem and higher brain regions. This communication pathway affects mood, cognition, and overall brain health. Dysregulation of the gut microbiota and serotonin levels in the gut can lead to alterations in vagal signaling, contributing to conditions such as depression and anxiety.
Research has increasingly focused on the role of gut health in depression, a condition often linked to low serotonin levels in the brain. Dysbiosis, or an imbalance in gut bacteria, may contribute to depressive symptoms by reducing serotonin production or impairing its signaling pathways. Studies show that gut microbiota can influence the development of depressive symptoms through changes in serotonin metabolism. Probiotic treatments aimed at restoring healthy gut bacteria have shown promise in alleviating depressive symptoms by modulating serotonin levels. A study published in the journal Psychiatry Research demonstrated that probiotic supplementation improved mood and reduced symptoms of depression in individuals with low serotonin levels .
Anxiety disorders are also associated with serotonin imbalances, both in the CNS and ENS. Gut bacteria influence serotonin production, which can have downstream effects on anxiety levels. The gut microbiota affects GABA, the brain's primary inhibitory neurotransmitter, and serotonin levels. Together, these neurotransmitters regulate emotional responses and stress resilience. Certain probiotic strains, such as Lactobacillus rhamnosus, have been shown to reduce anxiety-like behavior by modulating serotonin and GABA production in the gut, according to a study in Proceedings of the National Academy of Sciences .
Irritable Bowel Syndrome (IBS) and Serotonin
IBS is a functional GI disorder characterized by abdominal pain, bloating, and altered bowel habits. Altered serotonin signaling in the ENS plays a major role in the pathophysiology of IBS, particularly in its diarrhea-predominant and constipation-predominant forms. In diarrhea-predominant IBS (IBS-D), there is an overproduction of serotonin, leading to increased gut motility and frequent bowel movements. Conversely, constipation-predominant IBS (IBS-C) is associated with reduced serotonin availability, leading to slower transit time through the intestines.
Emerging evidence suggests a link between serotonin dysregulation in the gut and autism spectrum disorder (ASD). Studies have shown that children with ASD often have elevated levels of serotonin in the blood (a condition known as hyperserotonemia), as well as significant alterations in their gut microbiota. Research published in Cell found that gut bacteria influenced serotonin levels in mouse models of autism, affecting social behavior and cognition . Preliminary studies indicate that modulating the gut microbiota with probiotics can improve behavioral symptoms in children with ASD, potentially by normalizing serotonin levels. Given the intricate relationship between gut microbiota, serotonin, and the nervous system, therapeutic strategies focusing on the gut-brain axis are gaining significant attention for managing serotonin-related disorders. These strategies aim to promote a healthy balance of gut bacteria, thereby influencing serotonin production and regulating mood, gut motility, and mental health. In this chapter, we will explore the therapeutic approaches available to modulate serotonin production in the gut and their broader impacts on the nervous system, including dietary interventions, probiotics, prebiotics, and emerging therapies.
Diet plays a crucial role in maintaining gut health and supporting serotonin synthesis. Since serotonin is synthesized from the amino acid tryptophan, a diet rich in tryptophan-containing foods is essential for optimal serotonin production. In addition to dietary tryptophan, several other dietary factors can support healthy gut microbiota, which in turn promotes serotonin regulation.
Foods high in tryptophan include turkey, chicken, eggs, fish, cheese, and nuts. These foods provide the necessary precursor for serotonin synthesis, both in the gut and brain. However, it’s important to note that simply increasing tryptophan intake may not be enough, as its availability for serotonin synthesis is influenced by various factors, including the presence of other amino acids and the gut’s ability to metabolize tryptophan.
A diet rich in fiber supports the growth of beneficial gut bacteria, which play a role in serotonin production. Fiber is fermented by gut bacteria into short-chain fatty acids (SCFAs), which, as mentioned earlier, promote serotonin release from enterochromaffin cells in the gut.
Found in fruits, vegetables, tea, and wine, polyphenols are plant compounds with antioxidant and anti-inflammatory properties. These compounds have been shown to positively influence gut microbiota composition, promote the growth of beneficial bacteria, and enhance serotonin signaling in the gut-brain axis. For example, polyphenol-rich foods like blueberries, grapes, and green tea are linked to improved cognitive function and mood, likely due to their impact on gut microbiota and serotonin production.
Certain individuals with gut disorders, such as irritable bowel syndrome (IBS), may benefit from a low-FODMAP diet. FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are poorly absorbed in the gut and can lead to bloating, gas, and discomfort. For individuals with serotonin dysregulation in the gut, such as those with IBS, reducing FODMAP intake may help regulate gut motility and serotonin-related symptoms like diarrhea or constipation.
Probiotics are live microorganisms that, when administered in adequate amounts, provide health benefits to the host, particularly by enhancing gut health and modulating neurotransmitter levels. Probiotics can directly influence serotonin production by promoting the activity of serotonin-producing gut bacteria or by enhancing the function of the enteric nervous system.
Lactobacillus and Bifidobacterium species: These beneficial bacterial strains have been shown to increase serotonin production by converting tryptophan into its metabolite forms, which can then be used for serotonin synthesis. Probiotic supplements containing these strains may help improve mood, reduce symptoms of anxiety, and support gut motility.
Research on Probiotics and Mental Health: A study published in the journal Gastroenterology found that supplementing with Lactobacillus rhamnosus improved emotional regulation and reduced symptoms of depression in individuals with gut dysbiosis. The authors attributed these benefits to the strain’s influence on serotonin pathways via the gut-brain axis .
Multi-Strain Probiotics: Probiotic supplements containing a combination of strains such as Lactobacillus acidophilus, Bifidobacterium longum, and others have shown promise in treating mood disorders linked to serotonin dysregulation. Multi-strain probiotics enhance gut microbial diversity, which is essential for maintaining healthy serotonin production.
Gut Microbiota and Anxiety: In addition to mood regulation, probiotics have demonstrated efficacy in reducing anxiety symptoms. A study published in Psychiatry Research found that individuals who took probiotics experienced significant reductions in anxiety symptoms, possibly due to the probiotics’ effect on gut serotonin production and vagal nerve activity .
Prebiotics are non-digestible fibers that promote the growth and activity of beneficial gut bacteria. Prebiotics are fermented by the microbiota into SCFAs like butyrate, which not only nourish the gut lining but also enhance serotonin production. Prebiotics, in combination with probiotics (a combination known as synbiotics), are increasingly being used to improve both gut health and mood.
Inulin and Fructooligosaccharides (FOS): These are two common prebiotics found in foods such as onions, garlic, leeks, asparagus, and bananas. They serve as a food source for beneficial bacteria like Bifidobacterium, which in turn promotes serotonin production.
Research on Prebiotics and Brain Function: A study in the journal Nutrients showed that prebiotic supplementation increased levels of beneficial bacteria, leading to improvements in cognition and mood by enhancing serotonin signaling along the gut-brain axis .
Galactooligosaccharides (GOS): GOS is another type of prebiotic that has been shown to positively influence gut health and serotonin production. It promotes the growth of specific bacteria involved in tryptophan metabolism, helping balance serotonin levels in the body.
The term psychobiotics refers to a class of probiotics and prebiotics that influence mental health through their action on the gut-brain axis. Psychobiotics modulate the gut microbiota, which in turn affects neurotransmitter levels, including serotonin, thereby influencing mood, stress responses, and cognitive function.
Mechanism of Action: Psychobiotics produce neuroactive compounds such as SCFAs, serotonin, and GABA. These compounds interact with the vagus nerve and the enteric nervous system, sending signals to the brain that influence emotional and cognitive processes.
Examples of Psychobiotics: Strains such as Lactobacillus rhamnosus and Bifidobacterium infantis have been identified as psychobiotics due to their ability to modulate serotonin and GABA production in the gut. Clinical trials have shown that these psychobiotics can alleviate symptoms of anxiety, depression, and stress .
The relationship between gut bacteria, serotonin, and the nervous system is a rapidly growing area of research. Scientists are increasingly recognizing the potential of gut-targeted therapies to treat mood disorders, gut-related diseases, and neurological conditions. Future research will likely focus on:
Microbial-Based Therapies: Advances in microbiome research could lead to the development of targeted microbial therapies that modulate serotonin production for the treatment of depression, anxiety, and cognitive decline.
Personalized Nutrition: With growing evidence of the gut-brain connection, personalized nutrition plans tailored to an individual’s microbiome could optimize serotonin production and support overall mental health.
Serotonin and Neurodegenerative Diseases: Research into how gut microbiota influence serotonin pathways may provide insights into treatments for neurodegenerative diseases like Parkinson’s and Alzheimer’s, where serotonin deficits are implicated.
Serotonin, a vital neurotransmitter, plays an integral role in both gut health and brain function. Its production is heavily influenced by the gut microbiota, which serves as a critical regulator of serotonin synthesis and signaling along the gut-brain axis. The interplay between serotonin and the gut microbiota has profound implications for mental health, mood regulation, and gastrointestinal function. Through dietary interventions, probiotics, prebiotics, and emerging therapies such as psychobiotics and FMT, we can modulate serotonin levels and improve both gut and brain health. The growing body of research underscores the importance of maintaining a healthy gut microbiome to ensure balanced serotonin production, ultimately supporting emotional well-being and cognitive function.
Chapter 6: Emerging Research and Future Directions
Serotonin, gut health, and the nervous system have become a focal point for research exploring the gut-brain axis and its broader implications for treating neurological and psychological disorders. Continued research into serotonin's modulation by gut bacteria will likely lead to advancements in treating diseases like depression, anxiety, and even neurodegenerative conditions. Future therapeutic strategies may involve personalized approaches, microbial-based therapies, and novel prebiotic and probiotic.
Herbs that Support the Enteric Nervous System
Due to the complexity of the ENS and its deep connection to digestive and emotional health, several herbs are commonly used to support its function. These herbs help regulate digestion, improve motility, reduce inflammation, and even influence neurotransmitter activity within the gut.
Peppermint (Mentha piperita) is one of the most widely used herbs for promoting gut health, particularly through its beneficial effects on the ENS. Peppermint contains menthol, a compound that relaxes the smooth muscles of the digestive tract, thus alleviating symptoms of irritable bowel syndrome (IBS) such as abdominal pain, bloating, and gas. Studies have demonstrated that peppermint oil, when encapsulated, can reduce the frequency of spasms and improve overall bowel function by acting on the calcium channels within the muscles of the intestines, making it a highly effective antispasmodic herb. This ability to ease muscle tension in the gut provides relief from the dysregulation of the ENS that characterizes IBS, a disorder where communication between the brain and the gut is often disrupted. Additionally, peppermint has anti-inflammatory properties, which help soothe the gut lining and reduce irritation, further enhancing its role in maintaining a balanced and healthy ENS.
Ginger (Zingiber officinale) is another potent herb that supports the ENS through its ability to promote gut motility and reduce inflammation. Ginger has been used for centuries in traditional medicine systems such as Ayurveda and Traditional Chinese Medicine to treat digestive issues ranging from nausea and indigestion to more severe conditions like gastritis. The active compounds in ginger, such as gingerols and shogaols, have been shown to stimulate gastric emptying and accelerate the movement of food through the GI tract, helping to alleviate symptoms of gastroparesis and constipation. By promoting efficient digestion and preventing the stagnation of food in the gut, ginger helps maintain the smooth operation of the ENS. Additionally, ginger’s anti-inflammatory and antioxidant properties help protect the gut lining from damage caused by excessive inflammation, a common issue in conditions like IBD, where the enteric nervous system's regulation of immune responses can become impaired. Research has also indicated that ginger may have prokinetic effects, improving the coordination of muscle contractions within the digestive tract, which is especially beneficial for individuals with dysregulated gut motility.
Chamomile (Matricaria chamomilla) is renowned for its calming effects on both the digestive and nervous systems, making it a key herb in supporting the ENS. Chamomile contains flavonoids and terpenoids, which provide potent anti-inflammatory and antispasmodic effects, helping to relax the muscles of the intestines and reduce cramping, bloating, and discomfort associated with digestive disorders like IBS. Beyond its physical effects on gut muscles, chamomile also acts on the central nervous system (CNS), promoting relaxation and reducing anxiety, which is often closely linked with digestive disorders through the gut-brain axis. Studies have shown that chamomile can reduce stress-induced GI symptoms by modulating the HPA (hypothalamic-pituitary-adrenal) axis, which in turn influences the ENS. This dual action of calming both the mind and the gut makes chamomile an ideal herb for addressing the psychosomatic aspects of GI conditions, where emotional stress exacerbates physical symptoms.
Another valuable herb for the ENS is licorice (Glycyrrhiza glabra), particularly its deglycyrrhizinated form (DGL), which has been shown to help protect the mucosal lining of the stomach and intestines. DGL licorice works by stimulating mucus production, which acts as a protective barrier in the gut, reducing irritation and allowing the tissues to heal from damage caused by acid reflux, ulcers, or inflammatory conditions like IBD. By reinforcing the gut lining, licorice helps prevent the breakdown of communication between the ENS and the digestive organs, ensuring that the neurons within the gut can function properly. Licorice also has anti-inflammatory properties, reducing the overactive immune response that often accompanies chronic gut disorders. Moreover, its soothing effects on the gut lining make it beneficial for individuals dealing with leaky gut syndrome, a condition where intestinal permeability is increased, leading to the translocation of toxins and inflammatory molecules into the bloodstream.
Slippery elm (Ulmus rubra) is another herb that is highly beneficial for the ENS due to its mucilaginous properties, which soothe and protect the gut lining. Slippery elm contains a high amount of mucilage, a gel-like substance that coats the walls of the intestines and helps to reduce irritation and inflammation. This protective layer not only shields the gut from further damage but also supports the regeneration of the gut lining, which can become compromised in conditions like ulcerative colitis and Crohn’s disease, both of which involve dysregulation of the ENS. Slippery elm’s ability to calm irritation in the gut helps restore balance to the ENS, reducing symptoms such as diarrhea, cramping, and bloating. By providing a protective coating, slippery elm also helps enhance nutrient absorption, supporting overall digestive health.
Fennel (Foeniculum vulgare) is another herb known for its positive effects on the ENS, particularly for reducing gas and bloating. Fennel contains compounds such as anethole, which act as carminatives, helping to expel gas from the intestines and reduce abdominal discomfort. This herb has been used traditionally to treat digestive disorders, including IBS, and its ability to relax the smooth muscles of the gut helps alleviate cramping and bloating associated with dysregulated gut motility. Additionally, fennel has mild anti-inflammatory effects, making it a soothing herb for those with sensitive stomachs or inflammation in the GI tract. Its impact on the ENS is further enhanced by its ability to stimulate the production of digestive enzymes, improving digestion and nutrient absorption.
In addition to these well-known herbs, marshmallow root (Althaea officinalis), turmeric (Curcuma longa), and dandelion (Taraxacum officinale) are also valuable for supporting the ENS. Marshmallow root, like slippery elm, is rich in mucilage and helps soothe the digestive tract by coating and protecting the gut lining. Turmeric’s active compound, curcumin, has potent anti-inflammatory effects that help reduce inflammation in the gut, making it beneficial for conditions like IBD. Curcumin has been shown to modulate gut motility and promote healing in the digestive tract by reducing inflammatory cytokines that disrupt ENS function. Dandelion, a natural bitter, stimulates bile production and supports liver function, which is closely tied to digestive health. Its mild laxative effect also helps promote regular bowel movements, preventing constipation and supporting the ENS.
In conclusion, herbs like peppermint, ginger, chamomile, licorice, slippery elm, and fennel offer natural and effective support for the enteric nervous system, addressing a range of digestive issues such as IBS, IBD, and other functional gut disorders. These herbs work by relaxing gut muscles, reducing inflammation, protecting the gut lining, and supporting healthy gut-brain communication. As research continues to uncover the profound connection between the ENS and overall health, these herbs remain valuable tools for maintaining digestive health and promoting the well-being of both the body and the mind.
Turmeric is known for its anti-inflammatory and antioxidant properties, and it has a protective effect on the digestive system. Curcumin, its active compound, helps reduce inflammation in the gut and may modulate neurotransmitter activity within the ENS. Turmeric reduces inflammation in the gastrointestinal tract, protecting the ENS from damage and promoting healthy digestion. It may also modulate serotonin production in the gut, which can alleviate symptoms of depression and anxiety. Clinical studies suggest that curcumin has a beneficial effect on both the enteric and central nervous systems, reducing symptoms of gastrointestinal disorders like IBS and improving mood .
Marshmallow root is another mucilaginous herb that helps soothe and protect the gut lining. It reduces irritation in the digestive tract and supports the healthy function of the ENS by calming inflammation and promoting healing. Marshmallow root coats the digestive tract with mucilage, reducing inflammation and protecting the ENS from irritation. Studies have shown that marshmallow root can reduce inflammation and promote healing in the gut lining, which is beneficial for maintaining the health of the ENS .
Lemon balm is known for its calming effects on both the nervous system and digestive system. It helps reduce anxiety and stress, which directly impacts the ENS, as stress often leads to digestive issues such as IBS. Lemon balm also improves digestive motility and reduces gas and bloating. Lemon balm calms the enteric nervous system by reducing stress and anxiety, improving digestive motility, and relieving symptoms like bloating and indigestion. Studies show that lemon balm can reduce anxiety-related digestive issues by modulating neurotransmitters in both the CNS and ENS .
HARVESTING OATS AT GAIA
Nerve Repair Herbs
Nerve damage can result from various causes, including injury, surgery, autoimmune diseases, and conditions like diabetes. Nerve damage in the brain and spinal cord is much more difficult to heal, while the PNS has a better capacity for regeneration. Over the years, several plants have been studied for their potential to support nerve repair, reduce inflammation, and promote the regeneration of damaged nerves.
Nerve damage can result from trauma, toxins, diabetes, autoimmune diseases, or neurodegenerative conditions like multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS). Symptoms of nerve damage can include pain, numbness, tingling, weakness, and in severe cases, loss of motor function. Nerves regenerate slowly, especially in the peripheral nervous system, which has a limited ability to heal itself.
Nerve repair involves multiple processes, including Neuroprotection: Protecting neurons from further damage. Neuroregeneration: Promoting the regrowth of axons and nerve fibers. Anti-inflammatory Action: Reducing inflammation, which exacerbates nerve damage. Neurotransmitter Modulation: Regulating neurotransmitter levels to facilitate communication between nerve cells.
Lion’s Mane is one of the most promising natural substances for nerve repair. It contains bioactive compounds like hericenones and erinacines that stimulate Nerve Growth Factor (NGF), which plays a crucial role in the growth, maintenance, and survival of neurons. Stimulates NGF production, enhances myelination (the insulation around nerves), and supports neuroplasticity. Studies show that Lion’s Mane can promote nerve regeneration in damaged peripheral nerves and improve cognitive function.
St. John’s Wort (Hypericum perforatum) ~ Traditionally used for its antidepressant properties, St. John’s Wort also shows promise in nerve repair due to its neuroprotective and anti-inflammatory properties. Inhibits the enzyme monoamine oxidase (MAO), increases serotonin levels, and reduces oxidative stress in neurons. Preclinical studies suggest that St. John’s Wort can help in the regeneration of damaged nerves and protect against neural cell death.
Ashwagandha (Withania somnifera) ~ Ashwagandha is a powerful adaptogen that helps the body cope with stress while also supporting nervous system health. It enhances nerve function and promotes nerve regeneration by reducing inflammation and oxidative stress. Modulates the release of stress hormones like cortisol, promotes neurogenesis (the growth of new neurons), and has anti-inflammatory properties. Studies show that ashwagandha improves nerve conduction and offers protection to the CNS.
Curcumin, the active compound in turmeric, is known for its strong anti-inflammatory and antioxidant properties. It plays a role in promoting nerve regeneration and protecting against further damage. Reduces oxidative stress, inhibits inflammatory cytokines, and promotes the survival of neurons by modulating NGF and BDNF (Brain-Derived Neurotrophic Factor). Curcumin has been shown to reduce inflammation in nerve tissues and enhance regeneration in animal models of nerve injury.
Ginkgo biloba is widely known for improving cognitive function by increasing blood flow to the brain, but it also has neuroprotective properties that support nerve repair. Improves circulation, enhances the supply of oxygen and nutrients to nerve cells, and has strong antioxidant effects. Studies show Ginkgo biloba can improve nerve function and recovery in peripheral nerve injury.
Gotu Kola is a well-known herb in Ayurvedic medicine, used for improving cognitive function and promoting nerve regeneration. It helps repair damage by promoting collagen production and improving circulation to damaged nerves. Enhances NGF levels, promotes collagen synthesis (important for the repair of nerve sheaths), and has anti-inflammatory effects. Clinical studies show that Gotu Kola improves recovery in nerve damage and supports cognitive function in patients with neurodegenerative diseases.
Bacopa Monnieri is traditionally used to enhance memory and cognitive function, but it also has neuroprotective properties. It reduces oxidative stress and inflammation in the brain and promotes the growth of new neurons. Modulates neurotransmitters like serotonin and acetylcholine, reduces oxidative stress, and stimulates NGF production. Bacopa has been shown to improve cognitive function and support the repair of damaged neurons.
Nettle seeds are rich in essential fatty acids, vitamins, and minerals that support nerve function and repair. They are also known for their adaptogenic properties, which help balance stress responses. Enhances nerve regeneration by reducing inflammation and oxidative stress, and supports adrenal health. Nettle seed has shown potential in neuroprotection and nerve regeneration.
Sources: PubMed - Nettle Seed and Nervous System Health
10. Skullcap (Scutellaria lateriflora)
Skullcap is known for its calming effects on the nervous system. It helps reduce inflammation in nerve tissues and promotes the regeneration of damaged nerves.
Mechanism: Acts as an antioxidant, reduces neural inflammation, and promotes the regeneration of damaged nerve fibers.
Research: Skullcap has been shown to have neuroprotective effects in studies of nerve damage.
Sources: Healthline - Skullcap Benefits
Butterfly Pea (Clitoria ternatea) and Mimosa Pudica for Nerve Repair
Butterfly Pea (Clitoria ternatea)
Butterfly pea, also known as blue pea, is a traditional Ayurvedic and Southeast Asian herb prized for its neuroprotective properties. Its primary benefits for nerve repair stem from its rich antioxidant content, particularly anthocyanins (the compounds responsible for its blue color) and flavonoids, which protect nerve cells from oxidative stress and promote regeneration.
Mechanisms Supporting Nerve Repair:
Neuroprotection: Butterfly pea’s high concentration of anthocyanins and flavonoids act as powerful antioxidants, which protect nerve cells from damage caused by free radicals. This is crucial in preventing neurodegeneration and promoting the healing of damaged nerves.
Research: Studies have shown that anthocyanins protect neurons and improve cognitive functions by reducing oxidative stress .
Neurogenesis and Memory Enhancement: Research on butterfly pea suggests it supports neurogenesis (the growth of new neurons), improves synaptic plasticity, and enhances memory. This is particularly beneficial in cases of nerve injury where regeneration is required.
Research: Animal studies have demonstrated that extracts of Clitoria ternatea can improve learning and memory by enhancing acetylcholine levels, which is essential for nerve communication and cognitive function .
Anti-inflammatory Effects: Inflammation exacerbates nerve damage, and butterfly pea contains bioactive compounds that inhibit pro-inflammatory enzymes and cytokines, creating a more favorable environment for nerve healing.
Research: Anti-inflammatory properties of butterfly pea have been observed in various studies, suggesting that it may help reduce neuroinflammation associated with conditions like neuropathy .
Uses:
Butterfly Pea Tea: Traditionally consumed as a tea, butterfly pea can be used for its calming and neuroprotective properties, aiding in nerve health over time.
Extracts and Powders: Concentrated extracts are available for use in supplements that aim to promote cognitive and neurological health.
Mimosa Pudica (Sensitive Plant)
Mimosa pudica, commonly known as the "sensitive plant" for its characteristic folding leaves when touched, has been used in traditional medicine to support the nervous system. Its healing properties are particularly relevant in nerve repair due to its anti-inflammatory, antioxidant, and neuroprotective effects.
Mechanisms Supporting Nerve Repair:
Nerve Growth and Regeneration: Mimosa pudica has been shown to enhance nerve regeneration, making it useful in the recovery of damaged nerves. Its role in improving neurogenesis has been attributed to its ability to promote healthy growth in nerve cells and axons.
Research: Studies suggest that extracts of Mimosa pudica stimulate axonal regeneration in cases of nerve injury, showing promise for use in peripheral nerve damage treatments .
Antioxidant Properties: The high levels of antioxidants in Mimosa pudica help neutralize oxidative damage, which is a leading cause of nerve cell degeneration. By scavenging free radicals, these antioxidants protect neurons and encourage repair.
Research: Studies indicate that antioxidants in Mimosa pudica help mitigate oxidative stress, which is crucial for the prevention and repair of nerve damage .
Anti-inflammatory Action: Chronic inflammation can delay nerve repair or exacerbate damage. Mimosa pudica contains compounds like alkaloids, flavonoids, and phenolics that exhibit significant anti-inflammatory properties, helping to create an environment conducive to nerve healing.
Research: Mimosa pudica’s anti-inflammatory properties have been demonstrated in various in vivo studies, supporting its use in conditions related to nerve inflammation .
Uses:
Mimosa Pudica Capsules and Tinctures: The plant is commonly available in supplement form and can be taken to support nerve health, particularly in recovery from nerve injuries or neurodegenerative conditions.
Topical Applications: In traditional medicine, pastes made from the leaves have been applied to affected areas to help alleviate nerve pain and promote healing.
Conclusion
Butterfly pea (Clitoria ternatea) and Mimosa pudica are two potent herbal remedies for nerve repair and neuroprotection. Both plants have shown significant promise in promoting nerve growth, protecting against oxidative damage, reducing inflammation, and improving overall nerve function. These herbs can be used as part of a holistic approach to treating nerve damage, whether from injury, degenerative diseases, or other neurological conditions.
References:
Anthocyanins in Butterfly Pea: PubMed - Neuroprotective Effects of Anthocyanins
Butterfly Pea on Cognitive Function: NCBI - Cognitive Benefits of Clitoria Ternatea
Anti-inflammatory Properties of Butterfly Pea: Journal of Inflammation Research
Mimosa Pudica and Nerve Regeneration: NIH - Mimosa Pudica and Axonal Regeneration
Neurogenesis with Mimosa Pudica: ScienceDirect - Nerve Regeneration and Mimosa Pudica
Antioxidant Properties of Mimosa Pudica: PubMed - Mimosa Pudica Antioxidants
Anti-inflammatory Effects of Mimosa Pudica: NCBI - Inflammation and Mimosa Pudica
11. Rhodiola Rosea: An adaptogen that reduces stress and protects neurons from oxidative damage.
Sources: PubMed - Rhodiola for Nerve Health
12. Holy Basil (Ocimum sanctum): Supports the nervous system by reducing stress and promoting neurogenesis.
Sources: NIH - Holy Basil
13. Lavender (Lavandula angustifolia): Calms the nervous system, reduces anxiety, and promotes nerve repair.
Sources: Healthline - Lavender for Stress and Nerve Health
14. Oatstraw (Avena sativa): Known for nourishing the nervous system and helping repair damaged nerves.
Sources: Herbal Academy - Oatstraw Benefits
15. Sage (Salvia officinalis): Protects neurons from oxidative stress and improves cognitive function.
Video ~ Tonic Plants for the Nervous System
PEACH
Anxiety & Panic Attacks
Properly Dosing Nervines
We need nervines daily in my opinion, and sometimes many times a day depending on our stress level. So many of us run on hyper drive, high anxiety, and chronically stressed. When you are recommending nervines to someone make sure you choose one of the more full proof nervines with low side effects, that can be taken in high doses. These can be used daily, and as often as every few hours. For serious panic higher doses than normal can be taken.
I find that tea when taken with calming breaths can be the most effective. If not taken with a moment of calm, tinctures generally work better if you are on the go. Doses are 2-6 droppers full in water, depending on the concentration of the tincture, and how badly the calming is needed. For higher levels of anxiety and stress, often higher doses are tolerated that normally could give a headache or belly discomfort. Someone can always add the tincture to water and then slowly sip, so their body is doing the final dosing around how much is consumed.
Full Proof Nervines for Stress Relief ~ Skullcap, Peach leaf and bark, Blue vervain, Ashwagandha, Catnip, Lemon balm, Linden
SKULLCAP HARVEST AT GAIA
Incredible Nervines for Cultivating Calm ~
Passionflower, Skullcap, Blue vervain, Motherwort, Tilo, Linden, Peach, Kava kava, Oatstraw, Valerian, St. John’s Wort, California poppy, Wild lettuce, Mugwort, White Peony, Lavender, Sage, Egyptain blue lotus, Cannabis (with correct dose), Elder flower, Rose, Wild cherry, Lemon balm, Chamomile, Ginger, Lemongrass, and the many others…
Lemongrass is a popular herb in traditional medicine known for its aromatic properties and soothing effects. It is commonly used to reduce stress, anxiety, and insomnia due to its calming influence on the nervous system. The essential oils extracted from lemongrass, particularly citral and myrcene, are believed to have anxiolytic (anxiety-reducing) effects, as well as potential mood-enhancing properties. Lemongrass contains compounds that may interact with GABA receptors in the brain, which play a key role in regulating mood and reducing neural excitability. By enhancing GABAergic activity, lemongrass can promote relaxation and reduce symptoms of anxiety.
The essential oils from lemongrass are often used in aromatherapy to promote relaxation. Studies show that inhaling lemongrass oil can reduce symptoms of stress and elevate mood, making it an effective tool for managing anxiety. Stress and anxiety are often accompanied by oxidative stress and inflammation. Lemongrass has strong antioxidant properties that protect the brain from oxidative damage, which can further reduce the physical symptoms associated with anxiety and stress.
A study published in the Journal of Alternative and Complementary Medicine found that the inhalation of lemongrass essential oil significantly reduced anxiety levels and improved autonomic responses in participants compared to a placebo group . Another study reported in the Journal of Ethnopharmacology demonstrated that lemongrass tea had a sedative effect, supporting its traditional use in treating anxiety and insomnia .
Tea: Drinking lemongrass tea is a common method for reducing stress and promoting relaxation. The tea is brewed from fresh or dried leaves and has a mild, pleasant flavor.
Essential Oil: Inhalation of lemongrass essential oil using a diffuser or applying it in diluted form to the skin can promote relaxation and ease anxiety.
Supplements: Lemongrass is available in capsule form, but it’s essential to follow dosage recommendations to avoid adverse effects.
Soursop Leaf (Annona muricata) for Stress and Anxiety
Soursop, also known as Graviola, is a tropical fruit known for its rich nutrient profile and medicinal properties. The leaves of the soursop tree have traditionally been used in herbal medicine to treat a wide variety of ailments, including stress and anxiety.
Soursop leaf extract contains bioactive compounds such as alkaloids and acetogenins that have been found to have sedative and anxiolytic properties. These compounds help reduce neural excitability and anxiety by modulating the brain’s neurotransmitter systems, including serotonin and GABA.
The leaf extract has also been studied for its adaptogenic properties, which help the body cope with stress. Adaptogens balance the body's stress response systems, preventing excessive cortisol production, which can lead to anxiety, depression, and fatigue. Soursop leaves contain antioxidants that protect the brain from oxidative stress, a condition that is often associated with chronic stress and anxiety. By reducing oxidative stress, soursop leaves may help improve mental clarity and reduce symptoms of anxiety.
A study published in the Journal of Pharmacognosy and Phytochemistry reported that soursop leaf extracts exhibited significant anxiolytic and sedative effects in animal models, supporting its traditional use for stress and anxiety relief . Another study published in the Journal of Medicinal Food confirmed the neuroprotective and calming effects of soursop leaf, suggesting its use as a natural remedy for anxiety disorders .
Tea: Soursop leaves are commonly used to make herbal teas, which can be consumed to reduce anxiety and promote relaxation. Simply steep the leaves in hot water for about 10-15 minutes before drinking.
Capsules or Extracts: Soursop leaf extract is also available in capsule or tincture form, which may be easier for those seeking a more concentrated dose.
Topical Application: Soursop leaf is sometimes used in traditional medicine as a topical treatment for muscle tension and stress-related physical discomfort.
Video ~ Nervines for Panic Attacks & Anxiety
PASSIONFLOWER
Soothing Depression
Depression is a common mental health condition affecting millions of people worldwide. While pharmaceutical treatments such as antidepressants are widely prescribed, many individuals seek natural remedies to complement or replace conventional treatments. Herbs have been used for centuries to alleviate mood disorders and provide relief from the symptoms of depression. This guide provides an in-depth exploration of various herbs that have shown promise in managing depression, supported by scientific studies and traditional use.
Depression is a mental health disorder characterized by persistent feelings of sadness, hopelessness, and a lack of interest in activities once enjoyed. It can also result in physical symptoms such as fatigue, changes in appetite, and difficulty sleeping. Depression is linked to imbalances in neurotransmitters such as serotonin, dopamine, and norepinephrine, which regulate mood and emotion.
Many causes of depression…
Nutritional deficiencies
Low omega 3 levels
Medications
Sugar
Not enough sunlight/ vit. D
Life events
Poor environment
Grief & loss
Negative environments and energy
Low energy or energy stagnation
Stress & Trauma
Hormonal imbalances
Neurotransmitter imbalances
Gut dysbiosis
Hypothyroidism
Toxin exposure
Heavy metals
Poor digestion
Candida or harmful gut bacteria overgrowth (bacteria release neuro-toxins that interfere with neurotransmitters)
Herbs for Situational Depression –
St. John’s Wort, Oatstraw, Schisandra, Lemon balm, Holy basil, Ashwagandha, Peach, Sweet Orange, California poppy, Skullcap, Blue vervain, Lavender, Rose, Cacao, Ginseng.
Trauma –
Rose, Marshmallow, Linden, Sage, Blue vervain, Motherwort, Evergreens (pine etc), Violet, Comfrey, Marshmallow, St. John’s Wort, Skullcap, Ashwagandha
Herbs for Neurotransmittor Imbalance related Depression –
Ashwagandha, St. John’s Wort, Schisandra, Holy basil, Rhodiola, Skullcap, Eleuthero (Siberian Ginseng), Gingko, Lemon balm, Ginseng
For Hormonal Depression –
Liver cleansing herbs (to help break down excess hormones), hormonal regulating herbs such as Red Raspberry, Red Clover, Vitex, Shatavari, Ashwagandha, adaptogens (endocrine balancing). Changes in diet, environment, cleansing/detox, digestive herbs & probiotics, omega 3s, cutting down on sugar, coffee, alcohol. Lowering stress levels.
Conventional Western Antidepressent Drugs ~ SSRIs work by blocking a receptor in the brains neural cells that reabsorbs the chemical serotonin, increasing the amount of serotonin available to pass from nerve cell to nerve cell.
MAOIs - Monoamine oxidase inhibitors - An enzyme called monoamine oxidase helps remove the neurotransmitters norepinephrine, serotonin and dopamine from the brain. MAOIs prevent this from happening, which makes more of these brain chemicals available.
Herbs work to treat depression by interacting with the body’s neurotransmitter systems, balancing hormones, and reducing inflammation. Many herbs offer fewer side effects than conventional antidepressants, making them a popular choice for individuals looking for natural alternatives.
Holy basil, also known as Tulsi, is another adaptogenic herb that helps reduce stress and improve mood. Holy basil reduces cortisol levels and improves neurotransmitter balance, helping to alleviate depression caused by stress. Studies show that holy basil can reduce the symptoms of anxiety and depression in patients with stress-related disorders .
Lemon balm is often used to reduce stress and anxiety, and it has been studied for its ability to improve mood and cognitive function. Lemon balm modulates neurotransmitters such as GABA and serotonin, which are involved in regulating mood.
Herbal remedies can often be combined to enhance their effects. Some combinations are particularly effective for managing the symptoms of depression:
One of the most well-known herbs for depression, St. John’s Wort is frequently used in Europe for mild to moderate depression. St. John’s Wort is believed to increase serotonin, dopamine, and norepinephrine levels by inhibiting their reuptake in the brain. This action is similar to that of selective serotonin reuptake inhibitors (SSRIs), a class of antidepressant drugs. It has been shown to improve mood, reduce anxiety, and alleviate symptoms of mild depression. St. John’s Wort can interact with many medications, including birth control pills, antidepressants, and blood thinners, so it should be used under medical supervision.
Rhodiola is an adaptogen, a type of herb that helps the body cope with stress and maintain balance. Rhodiola is thought to influence the regulation of serotonin, dopamine, and norepinephrine, helping to support overall neurotransmitter balance. It may also reduce cortisol levels, the body’s primary stress hormone. Studies suggest that Rhodiola can improve mood, reduce fatigue, and enhance cognitive function, making it helpful for people with depression or stress-related mood disorders. While generally safe, it may cause side effects like dizziness or dry mouth in some individuals.
Another adaptogenic herb, ashwagandha is known for its ability to reduce stress and anxiety while promoting emotional balance. Ashwagandha reduces cortisol and supports the regulation of GABA (gamma-aminobutyric acid), a calming neurotransmitter. It may also influence serotonin and dopamine pathways, helping to stabilize mood. Research suggests ashwagandha can reduce symptoms of anxiety, improve sleep, and enhance overall well-being in people with stress-related mood issues. Ashwagandha is generally safe, though it can cause mild digestive upset in some people.
Ginkgo is primarily known for improving cognitive function, but it may also have antidepressant effects. Ginkgo is thought to enhance blood flow to the brain and support the regulation of serotonin and dopamine levels, which are critical for mood stabilization. Some studies suggest Ginkgo can reduce symptoms of depression, especially in elderly individuals or those with cognitive decline. Ginkgo can interact with blood thinners and other medications, so it should be used cautiously.
Turmeric, particularly its active compound curcumin, has powerful anti-inflammatory and antioxidant properties that may benefit mental health. Curcumin is believed to increase levels of brain-derived neurotrophic factor (BDNF) and serotonin, both of which play roles in mood regulation. It also helps reduce inflammation, which has been linked to depression. Studies suggest curcumin supplementation may help improve symptoms of depression, particularly when combined with conventional antidepressant medications. Turmeric is generally safe, but it may interact with blood-thinning medications or cause gastrointestinal issues in high doses.
Lavender is commonly used in aromatherapy, but it can also be taken orally to help alleviate anxiety and depression. Lavender appears to have calming effects, likely through modulation of GABA, serotonin, and dopamine. It’s thought to have anxiolytic and mood-stabilizing properties. Clinical studies have shown that lavender can reduce anxiety and improve sleep quality, both of which are important for managing depression. Lavender is safe for most people, though it can cause allergic reactions in some individuals.
Passionflower is often used to reduce anxiety and improve sleep, but it also has mild antidepressant properties. Passionflower increases GABA levels, which has a calming effect on the brain. This can help reduce symptoms of anxiety and mild depression. It’s particularly helpful for people who experience both anxiety and depression, and it can improve overall sleep quality.
Chamomile is well-known for its soothing effects and is often used to reduce anxiety and promote relaxation. Chamomile may work by modulating GABA receptors, similar to how certain anti-anxiety medications function. It also has mild antidepressant effects. Chamomile is useful for reducing anxiety and symptoms of mild depression, especially when related to stress or insomnia.
Herbs such as St. John’s Wort, Rhodiola, Ashwagandha, and others offer natural options for supporting mood and balancing neurotransmitters like serotonin, dopamine, and GABA. These herbs can be beneficial for mild to moderate depression, anxiety, and overall mental health support. However, it’s important to use them under the guidance of a healthcare provider, especially if taking other medications, to avoid interactions and side effects.
Video ~ Plants for Depression & Joy
Brain Health
Improving Cognition, Memory, and Concentration
Dementia, Alzheimers & Memory Loss
ADHD
Manic Depression & Bipolar
Schizophrenia
Herbs for Brain Repair: A Comprehensive Guide
The human brain is a remarkable organ with the ability to adapt, heal, and regenerate. However, various factors like aging, trauma, neurodegenerative diseases, and oxidative stress can hinder its ability to function optimally. In recent years, interest in natural remedies, particularly herbs, for supporting brain health and repair has grown. Several herbs are known for their neuroprotective properties, and they play a role in promoting neurogenesis, reducing inflammation, and protecting brain cells from damage. In this guide, we will explore a wide range of herbs that have been studied for their brain-repairing properties, supported by scientific evidence and traditional uses.
Brain repair primarily involves neuroplasticity and neurogenesis. Neuroplasticity is the brain’s ability to reorganize itself by forming new neural connections, while neurogenesis refers to the growth of new neurons, especially in the hippocampus, the area involved in learning and memory.
The brain can be damaged by various factors, including concussions, strokes, and other brain injuries.
Oxidative Stress: Free radical damage caused by environmental factors and aging.
Neuroinflammation: Chronic inflammation can degrade brain cells over time, contributing to cognitive decline.
Neurodegenerative Diseases: Conditions like Alzheimer’s, Parkinson’s, and Huntington’s disease cause progressive brain damage.
Herbs can support brain repair by reducing inflammation, protecting against oxidative damage, and encouraging neurogenesis.
Lion’s Mane mushroom is one of the most powerful natural remedies for brain health. It contains bioactive compounds like hericenones and erinacines, which have been shown to stimulate nerve growth factor (NGF), a protein essential for the growth, maintenance, and survival of neurons. Promotes neurogenesis, supports myelination, and improves synaptic plasticity.
Ginkgo Biloba is known for improving blood circulation in the brain and protecting neurons from oxidative stress. It has long been used to improve memory and cognitive function. Enhances blood flow to the brain, has antioxidant properties, and protects against free radical damage.
Gotu Kola has been used in Ayurvedic and Traditional Chinese Medicine for centuries to support brain function and repair. It is believed to enhance cognitive function, promote neurogenesis, and improve circulation. Stimulates NGF production, enhances synaptic plasticity, and has anti-inflammatory effects. A 2016 study found that Gotu Kola improved cognitive function and memory retention in individuals with cognitive decline .
Ashwagandha is an adaptogenic herb that helps reduce stress and anxiety, but it also has neuroprotective properties that support brain repair. It has been shown to promote neurogenesis and protect brain cells from damage. Modulates cortisol levels, promotes neurogenesis, and protects neurons from oxidative damage. A study published in the Journal of Dietary Supplements found that Ashwagandha improved cognitive function and promoted neuron growth in animal models .
Turmeric, and its active compound curcumin, is widely known for its potent anti-inflammatory and antioxidant properties. It protects brain cells from oxidative stress and promotes the regeneration of neural cells. Reduces inflammation, promotes the production of BDNF (Brain-Derived Neurotrophic Factor), and protects against oxidative stress. A 2018 study found that curcumin improved memory and attention in individuals with mild memory complaints .
Rhodiola is an adaptogen that helps reduce stress and fatigue while improving cognitive function. It enhances the body's resilience to stress, which is crucial for preventing brain damage. Enhances serotonin and dopamine levels, reduces stress-induced damage to neurons, and protects against cognitive decline. Studies have shown that Rhodiola improves cognitive function and reduces symptoms of fatigue and depression in individuals with chronic stress .
Ginseng is a traditional herb known for its neuroprotective effects. It improves brain function, boosts memory, and protects neurons from damage caused by aging and oxidative stress. Increases blood flow to the brain, protects neurons from oxidative stress, and promotes neurogenesis. A study published in Neuroscience Letters found that Ginseng improved cognitive function and enhanced memory in elderly individuals.
Sage has long been used for its cognitive-enhancing properties, especially in improving memory and concentration. It also has antioxidant properties that protect the brain from oxidative stress. Inhibits the breakdown of acetylcholine, a neurotransmitter important for memory, and has antioxidant effects.
Rosemary is another herb traditionally used to enhance memory and cognitive function. It contains compounds that protect neurons and improve brain circulation. Improves circulation, has antioxidant properties, and protects against free radical damage.
Herbs like Lion’s Mane, Gotu Kola, Ashwagandha, and Bacopa are particularly effective in promoting neurogenesis, the process of generating new neurons. These herbs work by increasing levels of growth factors like NGF and BDNF, which are essential for brain repair and recovery.
Chronic inflammation is one of the major contributors to neurodegeneration. Herbs such as Turmeric, Ginseng, and Rhodiola have potent anti-inflammatory properties, making them ideal for supporting brain health and preventing cognitive decline.
Herbs for Addiction
Addiction is a complex and chronic condition characterized by the compulsive use of substances such as alcohol, nicotine, or drugs, despite harmful consequences. It involves changes in the brain’s reward system, resulting in cravings, withdrawal symptoms, and an inability to control consumption. While conventional treatments for addiction include medications, counseling, and support groups, many individuals seek complementary therapies, including the use of herbs, to support recovery. Herbs can help reduce cravings, ease withdrawal symptoms, and promote mental and emotional healing.
This guide explores various herbs that have been traditionally and scientifically studied to assist with addiction recovery. It covers their mechanisms of action, how they aid in the recovery process, and their traditional uses.
Chapter 1: Understanding the Role of Herbs in Addiction Recovery
The Physiology of Addiction
Addiction affects the brain’s neurotransmitter systems, particularly dopamine, which plays a key role in the brain’s reward system. Substances of abuse cause excessive release of dopamine, leading to feelings of euphoria. Over time, the brain’s natural ability to produce dopamine decreases, making individuals reliant on the substance to feel pleasure. Withdrawal symptoms can range from physical discomfort to intense psychological distress.
Addiction is a complex condition involving physical, psychological, and neurological factors, making treatment and recovery particularly challenging. Traditional approaches to addiction treatment often involve medications, behavioral therapies, and support systems like counseling and rehabilitation programs. However, a growing body of research is exploring the use of herbal remedies to support addiction recovery. Herbs have been used for centuries in various traditional medical systems, such as Ayurveda and Traditional Chinese Medicine (TCM), to promote physical and mental well-being, reduce withdrawal symptoms, and balance neurotransmitters. This paper will discuss several herbs that have shown promise in supporting addiction treatment and recovery, including Kudzu, Milk Thistle, St. John’s Wort, Ashwagandha, Passionflower, Rhodiola, and Ginseng, among others.
Kudzu (Pueraria lobata)
Kudzu, a vine native to China and Japan, has been traditionally used in Chinese medicine to reduce alcohol consumption and curb cravings. The active compounds in Kudzu, particularly puerarin, daidzin, and daidzein, are believed to affect alcohol metabolism and reduce the desire for alcohol. Research has shown that Kudzu extract can reduce alcohol intake by modulating neurotransmitter pathways, particularly those involving dopamine, which plays a key role in the brain's reward system. By reducing the release of dopamine in response to alcohol, Kudzu helps diminish the reinforcing effects of alcohol, thereby lowering the likelihood of excessive consumption. Clinical studies have demonstrated that individuals who took Kudzu extract experienced reduced alcohol cravings and drank less compared to those on a placebo. This suggests that Kudzu may be a valuable herb in managing alcohol dependency and promoting recovery.
Milk Thistle (Silybum marianum)
Milk Thistle is well-known for its liver-protective properties, making it a valuable herb for individuals recovering from alcohol or drug addiction. Chronic substance abuse, particularly alcohol and certain drugs, can lead to liver damage. Milk Thistle’s active ingredient, silymarin, has been shown to support liver regeneration and protect liver cells from toxins. It acts as an antioxidant, reducing oxidative stress, which is often exacerbated by addiction and substance withdrawal. By enhancing liver function, Milk Thistle not only aids in detoxification but also promotes overall recovery by helping the body eliminate toxins more effectively. Some studies have even suggested that Milk Thistle may enhance recovery by reducing cravings and improving mood, likely due to its liver-regenerating properties, which help restore balance in the body during detoxification.
St. John’s Wort (Hypericum perforatum)
St. John’s Wort is commonly used for treating depression and anxiety, but it also has potential in addiction recovery. Addiction often co-occurs with mood disorders, and St. John’s Wort's effects on neurotransmitters, particularly serotonin, may help regulate mood and reduce the emotional triggers that lead to substance use. By increasing serotonin levels, St. John’s Wort can improve mood stability and reduce feelings of anxiety and depression, which are common during withdrawal and early recovery. Additionally, some studies suggest that St. John’s Wort may have mild effects on dopamine and norepinephrine, both of which are involved in the brain's reward system and are disrupted in individuals with addiction. Though more research is needed, the herb’s ability to balance mood and neurotransmitter activity makes it a valuable supplement in holistic addiction recovery protocols.
Ashwagandha (Withania somnifera)
Ashwagandha, a prominent herb in Ayurvedic medicine, is known for its adaptogenic properties, which help the body manage stress and restore balance in the nervous system. Addiction recovery is often marked by high levels of stress and anxiety, which can lead to relapse if not properly managed. Ashwagandha works by modulating the hypothalamic-pituitary-adrenal (HPA) axis, reducing cortisol levels, and promoting relaxation without sedation. Its effects on the GABA system, the brain's main inhibitory neurotransmitter, make it useful in reducing anxiety and promoting calmness, which are essential during withdrawal and recovery. Additionally, Ashwagandha has neuroprotective properties, reducing oxidative stress in the brain and supporting neurotransmitter balance. Studies have shown that Ashwagandha can help alleviate withdrawal symptoms, reduce cravings, and improve overall mental well-being, making it a valuable herb in the context of addiction recovery.
Passionflower (Passiflora incarnata)
Passionflower has been used for centuries as a natural remedy for anxiety, insomnia, and nervous disorders, all of which are common during addiction recovery. The herb works by increasing GABA levels in the brain, promoting relaxation and reducing feelings of anxiety and agitation. Passionflower has been found to be especially helpful in managing the symptoms of opioid and benzodiazepine withdrawal, both of which are known for their intense withdrawal syndromes. In clinical studies, Passionflower has been shown to reduce the severity of withdrawal symptoms, particularly anxiety and agitation, without causing sedation or dependence. Its calming effects make it a supportive herb for individuals going through detoxification and early recovery when withdrawal symptoms are at their peak.
Rhodiola (Rhodiola rosea)
Rhodiola, another adaptogenic herb, has been widely studied for its ability to reduce fatigue, enhance mental clarity, and improve mood. Addiction, particularly to stimulants like cocaine or methamphetamines, can severely deplete the body's energy reserves and impair cognitive function. Rhodiola helps restore energy levels by supporting the body's stress response and enhancing dopamine and serotonin activity in the brain. By improving neurotransmitter balance, Rhodiola can help reduce the cravings and fatigue associated with stimulant withdrawal. Additionally, Rhodiola has been shown to reduce symptoms of depression and anxiety, making it a useful herb for individuals recovering from addiction, where mood stabilization is critical for long-term success.
Ginseng (Panax ginseng)
Ginseng is a well-known adaptogen with powerful effects on physical and mental stamina, making it particularly useful in addiction recovery, where individuals often experience fatigue, low motivation, and cognitive impairment. Ginseng has been shown to increase dopamine and norepinephrine levels, helping to restore motivation and focus, which are often diminished during addiction and withdrawal. By enhancing these neurotransmitters, Ginseng can help combat the "reward deficiency" often seen in individuals with addiction, where everyday activities fail to trigger the same pleasure or motivation as drugs or alcohol. Studies have suggested that Ginseng may reduce cravings and withdrawal symptoms, especially for individuals recovering from stimulant addiction. Its ability to improve mental clarity and physical resilience makes it a strong candidate for supporting long-term recovery.
Valerian (Valeriana officinalis)
Valerian is another herb with potent calming properties, often used to treat insomnia and anxiety. During addiction recovery, especially in the detoxification phase, sleep disturbances and restlessness are common. Valerian works by enhancing GABA transmission, promoting relaxation and improving sleep quality without the risk of dependence that often accompanies pharmaceutical sedatives. By promoting rest, Valerian helps individuals going through withdrawal manage stress and physical symptoms more effectively. In addition to its benefits for sleep, Valerian has been studied for its ability to reduce the intensity of withdrawal symptoms in individuals recovering from opioids, alcohol, and benzodiazepines.
Lobelia (Lobelia inflata)
Lobelia has a long history of use in traditional medicine, particularly for treating respiratory conditions. However, it has also been used in addiction treatment, especially for nicotine withdrawal. Lobelia contains an alkaloid called lobeline, which is thought to mimic some of the effects of nicotine, reducing cravings and withdrawal symptoms in individuals trying to quit smoking. Lobeline may also act on dopamine receptors, helping to alleviate the reward deficiency associated with quitting nicotine. Although Lobelia is often used in combination with other therapies for smoking cessation, it shows promise as a natural aid for reducing cravings and supporting the detoxification process.
Holy Basil (Ocimum sanctum)
Holy Basil, another adaptogenic herb used in Ayurvedic medicine, is known for its stress-relieving properties and ability to balance neurotransmitters. Chronic stress is a major trigger for substance use, and Holy Basil works by reducing cortisol levels and enhancing serotonin and dopamine activity in the brain. This helps to reduce anxiety and depression, both of which are common in individuals recovering from addiction. Holy Basil also has antioxidant properties that protect the brain and body from the oxidative stress caused by chronic substance abuse. By supporting emotional balance and reducing stress, Holy Basil helps individuals maintain sobriety and prevent relapse during recovery.
Conclusion
The use of herbs in addiction treatment offers a promising complementary approach to conventional therapies. Herbs like Kudzu, Milk Thistle, St. John’s Wort, Ashwagandha, Passionflower, Rhodiola, Ginseng, Valerian, Lobelia, and Holy Basil work by balancing neurotransmitters, reducing withdrawal symptoms, and promoting emotional and physical resilience. While more research is needed to establish standardized dosages and long-term efficacy, these herbs show significant potential in helping individuals recover from addiction. As part of a holistic recovery program, herbs can provide natural support for the body and mind, aiding in detoxification, mood stabilization, and overall well-being. However, individuals should always consult healthcare providers before incorporating herbs into their recovery plan, particularly when combined with other medications or therapies, to ensure safety and effectiveness.
Skullcap (Scutellaria lateriflora) is another herb that has shown promise in the context of addiction treatment, particularly for its calming and anxiety-reducing properties. Skullcap has been used traditionally in herbal medicine as a nervine tonic, meaning it helps to soothe the nervous system, which is highly beneficial during the withdrawal phase of addiction recovery. Withdrawal from substances such as alcohol, opioids, or nicotine often results in heightened anxiety, agitation, and insomnia—symptoms that can increase the risk of relapse. Skullcap works by modulating GABA (gamma-aminobutyric acid) receptors, which are involved in reducing excessive brain activity and promoting a state of relaxation. By enhancing GABAergic activity, skullcap helps reduce withdrawal-related anxiety and tension, allowing individuals in recovery to feel more emotionally stable and calm.
Additionally, skullcap possesses antioxidant and anti-inflammatory properties, which can be beneficial for detoxifying the body and protecting brain cells from oxidative stress caused by prolonged substance abuse. Studies suggest that skullcap may also reduce cravings and help balance mood by influencing dopamine and serotonin pathways, two neurotransmitters that play key roles in the brain's reward system and are often dysregulated in addiction. Although more research is needed to fully understand the specific mechanisms through which skullcap can support addiction recovery, its calming effects and ability to stabilize mood make it a valuable herbal remedy in holistic treatment approaches, particularly for individuals dealing with high levels of stress and anxiety during the early stages of sobriety.
HIBISCUS
Antioxidants to Protect
The Brain & Nervous System
Antioxidants are molecules that neutralize free radicals, reducing oxidative damage and promoting cell repair. They act by donating electrons to stabilize free radicals, thus preventing these unstable molecules from causing further damage to cells. By incorporating foods and herbs rich in antioxidants, you can support brain repair and protect the nervous system from oxidative damage.
The brain, despite being only about 2% of the body's weight, consumes approximately 20% of its oxygen. This high demand for oxygen also makes the brain highly susceptible to oxidative stress, which is caused by an imbalance between the production of harmful free radicals and the body's ability to detoxify them. Oxidative stress is a major contributor to neurodegenerative diseases such as Alzheimer's, Parkinson's, and Huntington's disease. Additionally, oxidative stress can accelerate the aging process and lead to cognitive decline. Antioxidants, which neutralize free radicals, play a crucial role in protecting and repairing brain cells.
In this guide, we will explore the importance of antioxidants for brain repair and the foods and herbs that provide these powerful nutrients. The science behind brain damage and repair mechanisms will also be discussed, followed by a detailed overview of specific antioxidants, herbs, and foods.
Oxidative stress occurs when there is an overproduction of reactive oxygen species (ROS) and reactive nitrogen species (RNS) that exceed the body's antioxidant defenses. In the brain, oxidative stress can damage neurons, leading to impaired cognitive function and the development of neurodegenerative diseases. Over time, oxidative stress results in the accumulation of lipid peroxidation, DNA damage, and protein oxidation, which collectively harm brain cells.
Antioxidant herbs and foods play a critical role in protecting the brain and nervous system from oxidative stress, which is a key factor in neurodegeneration and cognitive decline. The brain is particularly vulnerable to oxidative damage due to its high demand for oxygen and fatty acids, making antioxidants essential for maintaining its health. Turmeric (Curcuma longa), with its active compound curcumin, is one of the most potent antioxidant herbs known for its neuroprotective effects. Curcumin neutralizes free radicals and reduces inflammation in the brain, potentially lowering the risk of neurodegenerative diseases like Alzheimer’s disease and Parkinson’s disease . Ginkgo biloba, another widely studied herb, enhances blood flow to the brain while offering strong antioxidant properties, which help protect neurons from oxidative damage and improve cognitive function .
Rosemary (Rosmarinus officinalis) is another herb rich in antioxidants, particularly carnosic acid, which has been shown to shield the brain from oxidative stress and prevent damage to nerve cells. Rosemary has been traditionally used to enhance memory and mental clarity, and research supports its potential to protect the brain from age-related cognitive decline . Blueberries are a superfood packed with antioxidants, particularly flavonoids, which have been shown to improve brain function and protect against oxidative stress. Studies suggest that regular consumption of blueberries can improve memory and delay brain aging by reducing oxidative damage to neurons . Similarly, green tea (Camellia sinensis) contains catechins, potent antioxidants that help reduce inflammation and protect the brain from oxidative stress, improving mental clarity and reducing the risk of neurodegenerative diseases .
Ashwagandha (Withania somnifera) is an adaptogen known for its antioxidant and neuroprotective properties, particularly in reducing oxidative stress in the brain. It helps lower levels of free radicals that can damage brain cells, promoting nerve regeneration and supporting cognitive function . Sage (Salvia officinalis) has also been shown to boost brain health due to its antioxidant properties, which protect the brain from damage and enhance memory and learning. Sage is particularly useful in reducing oxidative stress and inflammation, two factors that contribute to the development of neurodegenerative diseases .
In the realm of antioxidant-rich foods, dark leafy greens like spinach and kale are abundant in vitamins A, C, and E, all of which serve as antioxidants that protect brain cells from oxidative damage. These vitamins also promote overall brain health by supporting cellular repair and reducing inflammation. Nuts, particularly walnuts, are rich in omega-3 fatty acids and antioxidants like vitamin E, which help fight oxidative stress and promote cognitive function . Goji berries and acai berries are also rich in antioxidants, particularly anthocyanins and polyphenols, which support brain health by reducing inflammation and protecting against oxidative damage.
By incorporating antioxidant-rich herbs and foods such as turmeric, ginkgo biloba, rosemary, blueberries, green tea, ashwagandha, and leafy greens into one’s diet, it is possible to significantly support brain and nervous system health, reduce the risk of cognitive decline, and promote overall mental clarity and resilience against neurodegenerative diseases.
Foods high. in beta-carotene (type of Vit. A) – Well-cooked red, yellow, or green vegetables/fruits: carrots, winter squash, tomatoes, seaweeds, cantaloupe, peppers & hot peppers, lettuce, kale, sweet potato, spinach, dandelion greens, mustard greens, cabbage, pumpkin, chard, collards, beet greens, lamb’s quarters, parsley, basil, squash, melons, peas, broccoli.
Herbs high in carotenes & carotenoids (helping to form Vit. A in the liver) –
F o o d s h i g h i n v i t a m i n C – Citrus, chili peppers, rose hips, bell peppers (esp. red), kale, broccoli, papaya, pineapple, strawberries, cauliflower, brussels sprouts, kiwi, mango.
H e r b s h i g h i n V i t a m i n C - Pine (evergreens), rose hips, yellow dock root, red clover, dandelion greens, plantain, parsley, schisandra, hibiscus, blueberry, strawberry, raspberry, nettles, purslane, violet, lambs’ quarters, marshmallow, sorrel, cayenne, paprika, parsley.
Essentail Fatty Acids = Flax oil, chia seeds, whole grains, borage oil, evening primrose oil, and all wild plants especially purslane.
Antioxidant Herbs (highest) – Clove, blueberry, billberry, cranberry, huckleberry, peppermint, rose, sage, garlic, ginger, turmeric, rosemary, peppermint, oregano, green tea, purslane, milk thistle, st. john’s wort, thyme, lemon balm, cinnamon, allspice, skullcap, triphala (ayurvedic blend), lady’s mantle, bearberry (uva ursi), birch, juniper needles & berries, pine, meadowsweet, marjoram.
Audio ~ Herbal Brain Tonics
DAMIANA
World of the Senses
& Movement
Somatic Experience
Our somatic nervous system also includes our sensory nervous system, which receives sensory information going from the body to the brain. Our motor nervous system is thought to be information sent from brain to skeletal muscles). These nerves also give us a sensory experience of the world.
Our somatic nervous system allows our body to move, and gives us the sensory experience that creates our experience of the world. This is our entire physical reality! Somatic nerves transmit impulses from our brain and spinal cord (central nervous system) to our skeletal muscle and creates our body movement. The nerves control all of our voluntary skeletal muscular systems within the body, which means our ability to walk, move, dance, and talk.
Movement has always been a delicious experience for me. I was a dancer for many years of childhood, which I still enjoy deeply. Some part of me has always known that we do not always have the ability to move well for our whole lives, and we have to take care of our body in order to continue to have free movement. Maybe it’s old soul memories of losing the function of some limbs, I don’t know… but I have a strong awareness that mobility is not something to take for granted. Many people with diseases or injuries that affect the nervous system or brain end up not have their full range of movement. Let us not take for granted what a gift it is to have full range of movement, and what support we can give people who have impairment of their body’s movement for a variety of reasons.
To support our body’s ability to move we have to address both our nervous system related issues that might be at play, as well as our musculoskeletal system. Some movement issues relate to nerve communication through our brain and spinal cord, or the peripheral nerves through our body coming from our spinal cord… and some movement issues relate more to what’s happening in our musculoskeletal system (such as joint impairment and inflammation).
The peripheral nervous system (PNS) includes all nerves and sensory neurons throughout the body, that are not in the brain or spinal cord. The PNS transmits information from body to the brain and spinal cord, as well as transmits information from the brain to the rest of the body. Sensory neurons run throughout the body and are most abundant and specialized in the hands, eyes, tongue, feet, ears, nose. These neurons are responsible for receiving and transmitting sensory information. Sensory nerve cells are responsible for converting external stimuli from the organism's environment into internal electrical impulses. The sensory information is sent to the brain, where the brain interprets it, and then the peripheral (motor) nervous system initiates responses.
The central nervous system is made of the brain and spinal cord. Carries sensory information to the brain from the PNS (Peripheral Nervous System). Conducts motor information to the effector organs - (reflexes). Brain - Site of cognitive (higher) functions: memory, learning, thinking. control of involuntary functions & control of voluntary functions o subconscious and emotions.
Herbs to Increase Sensory Information ~
Kava kava, mugwort, skullcap, sage, egyptian blue lotus, wild lettuce, damiana, elder flower, cannabis, psilocybin mushrooms, calamus, mints, ylang ylang, aphrodisiacs!
Herbs for Nerve Pain
Herbs have long been used to alleviate nerve pain, also known as neuropathic pain, which occurs due to damage or dysfunction of the nervous system. Unlike other types of pain, nerve pain can be particularly challenging to treat and may involve sensations such as burning, tingling, or shooting pain. Several herbs have shown promise in managing nerve pain by reducing inflammation, soothing the nervous system, and promoting nerve regeneration. St. John’s Wort (Hypericum perforatum) is one such herb that has been traditionally used for its anti-inflammatory and nerve-calming properties. It has been found to promote the healing of damaged nerves and reduce neuropathic pain, likely due to its ability to modulate the neurotransmitter GABA, which helps reduce pain signals.
Turmeric (Curcuma longa), with its active compound curcumin, is another potent herb for nerve pain. Curcumin has powerful anti-inflammatory and antioxidant effects, which can help reduce inflammation and oxidative stress around damaged nerves, easing pain. Cayenne pepper (Capsaicin) contains capsaicin, a compound known for its ability to reduce pain by depleting substance P, a chemical involved in transmitting pain signals. Topical creams containing capsaicin are often used to alleviate nerve pain, especially in conditions like diabetic neuropathy.
Skullcap (Scutellaria lateriflora) is another herb known for its ability to calm the nervous system and alleviate nerve-related pain. It acts as a nervine, reducing anxiety and helping soothe overactive nerve signals, which can be particularly beneficial in conditions like sciatica or nerve compression. Willow bark (Salix alba) contains salicin, which is converted into salicylic acid in the body and has pain-relieving effects similar to aspirin. It is commonly used to reduce inflammation and pain, including nerve-related pain. Lastly, Valerian root (Valeriana officinalis) is well-known for its muscle-relaxing and nerve-soothing properties, making it helpful for managing nerve pain associated with muscle tension and spasms. Collectively, these herbs offer natural alternatives to managing nerve pain by addressing inflammation, nerve damage, and pain signals, helping to restore balance to the nervous system.
Herbs have been used for centuries to alleviate various forms of body pain, offering a natural alternative to pharmaceutical medications. Several herbs possess anti-inflammatory, analgesic, and muscle-relaxing properties that can help ease chronic pain, muscle aches, and joint discomfort. Turmeric (Curcuma longa), widely known for its active compound curcumin, is one of the most powerful natural anti-inflammatory herbs. Curcumin works by inhibiting inflammatory pathways in the body, making it highly effective in reducing pain associated with conditions like arthritis and muscle sorenesser officinale)** also possesses potent anti-inflammatory and antioxidant effects. Studies have shown that it can reduce pain and stiffness, particularly in patients with osteoarthritis and rheumatoid arthritis, by reducing levels of pro-inflammatory cytokines .
Another herb,x alba)**, has been used historically as a natural source of salicin, which is chemically similar to aspirin. Willow bark acts as an analgesic and anti-inflammatory agent, and is commonly used to relieve pain from backaches, arthritis, and muscle strains . **Boswellia (Boswellia serrata)*an frankincense, has shown remarkable efficacy in treating pain and inflammation. Its active components, boswellic acids, inhibit inflammatory enzymes, making it a strong remedy for joint pain, particularly in conditions like osteoarthritis .
Devil's Claw (Harpagophytum procumbens) is ab for reducing body pain, especially lower back pain and arthritis. The active compounds, harpagosides, have strong anti-inflammatory and pain-relieving properties, comparable to nonsteroidal anti-inflammatory drugs (NSAIDs) . Additionally, Capsaicin, the active compound found in Cayenne um), is commonly used in topical treatments for pain. Capsaicin works by depleting substance P, a chemical in nerve cells responsible for transmitting pain signals, and is effective for managing conditions like muscle pain, joint pain, and nerve pain .
Arnica (Arnica montana) is another herb widely used for its anti-inflammatory and ticularly in treating bruises, muscle pain, and sprains. It is often applied topically in creams and ointments to reduce pain and swelling . Feverfew (Tanacetum parthenium) has been traditionally used to treat headaches and migraine painparthenolide**, which inhibits serotonin release and helps prevent blood vessel constriction, thereby reducing headache intensity and frequency .
Lastly, Valerian Root (Valeriana officinalis) and Skullcap (Scutellaria lateriflora), both recognized for their muscleare particularly useful in treating muscle tension and spasms, as well as reducing overall body pain. Valerian root, in particular, works by increasing levels of gamma-aminobutyric acid (GABA), a neurotransmitter that calms the nervous system and reduces pain perception . Together, these herbs offer a natural, effective approach to managing body pain by targeting inflammation, relaxing muscles, and blocking pain
St. John’s Wort is commonly known for its antidepressant properties, but it is also effective in treating nerve pain and neuralgia. It has been traditionally used to treat sciatica, nerve injuries, and neuropathic pain. St. John’s Wort modulates serotonin, dopamine, and norepinephrine levels, which can help alleviate nerve pain. It also has mild anti-inflammatory properties.
Skullcap is an herb known for its calming effects on the nervous system. It is used to alleviate nerve pain, muscle spasms, and tension headaches. Skullcap contains flavonoids such as baicalin, which has neuroprotective and anti-inflammatory properties. It calms overactive nerves and reduces the sensation of pain. Research has shown that skullcap reduces nerve excitability and has an overall calming effect on the nervous system.
Passionflower is known for its calming properties and is often used to treat anxiety, insomnia, and nerve pain. It has been traditionally used to treat neuralgia and conditions like fibromyalgia. Passionflower increases GABA (gamma-aminobutyric acid) levels in the brain, which helps reduce nerve excitability and pain. Studies published in the Journal of Clinical Pharmacy and Therapeutics show that passionflower reduces neuropathic pain and improves sleep quality in individuals with nerve pain .
The Sensory World
ROSEMARY